Where Have All the Patients Gone? The Art and Soul of Recapturing Lost Treatment Volume
October 23, 2020 | By Scot Latimer and David W. Johnson
On a plane trip to Oberlin College in October 1955, singer Pete Seeger wrote the first three verses of the popular anti-war song Where Have All the Flowers Gone? With a haunting tune, the song moves from flowers to young girls to soldiers to graveyards and back to flowers. Each verse ends with the provocative refrain, “When will they ever learn? When will they ever learn?”
As American society reopens, healthcare providers are asking themselves a version of those original questions: “Where have all the pre-COVID patients gone?”
Among the many “new normals” in post-COVID healthcare is the significant loss of patient volume at hospitals, clinics, and emergency departments along with dramatic increases in virtual care. In this sense, COVID-19 may be fundamentally altering healthcare supply-demand dynamics with far-reaching consequence for healthcare providers.
The financial losses associated with lower patient volumes throughout the pandemic have been catastrophic. The infusion of emergency funding to hospitals through the CARES Act has mitigated operating losses, but long-term sustainability requires a normalization of treatment activity. All providers are now scrambling to recapture lost patient volume.
Unfortunately, bringing patients back to healthcare facilities is proving more daunting than most providers expected. An “open and they will come” operating orientation isn’t working. Changing supply-demand dynamics may explain some of the lost volume: lost insurance coverage; the appeal of virtual and urgent care modalities; less pursuit of low-value care.
A more troubling and determinative reason for lower patient volumes is that consumers have lost confidence in healthcare providers. Gensler undertook a major 50-city pulse survey in Spring of 2020 “to understand how the global pandemic is influencing attitudes, decision-making, experiences, and expectations for healthcare.”
The news isn’t good. The survey found that 35% of respondents have reduced confidence in the overall health system. These respondents have less trust that the health system “will keep them safe from infection or other harm.”
Human beings are not machines. Receiving healthcare services is intensely personal. Emotions and experience influence healthcare decision-making, perhaps now more than ever. Neglecting their fears and preferences alienates patients. Many choose not to engage. When that happens, everyone loses.
Regaining consumer confidence begins with the humbling acknowledgement that healthcare delivery often fails to be “humane” by not acknowledging and accommodating individual needs, fears and preferences. It continues with a sincere determination to reconfigure and personalize the full care delivery experience.
The good news is that investment in humane healthcare today will pay big future dividends as healthcare becomes more consumer-centric and retail-oriented. The technology for mass customization of visits already exists. When will health systems ever learn? The time to do so is now.
The COVID Conundrum
As the healthcare industry adjusts to a “new normal” operating environment, it must explore how and why patient volume has shifted during the pandemic.
Last May, Strata Decision Technology launched The National Patient and Procedure Tracker to assess the impact of COVID-19 on hospital treatment volume. Their initial analysis across 40 states and 228 hospitals found that unique patients declined 54.5% between March 24th and April 6, 2020, compared to the equivalent period in 2019.
This volume decline occurred in both inpatient and outpatient settings across all disease categories. Cardiology encounters dropped 57%. Stroke treatments dropped 56%. Cancer procedures dropped 37%. Emergency department visits dropped 50%.
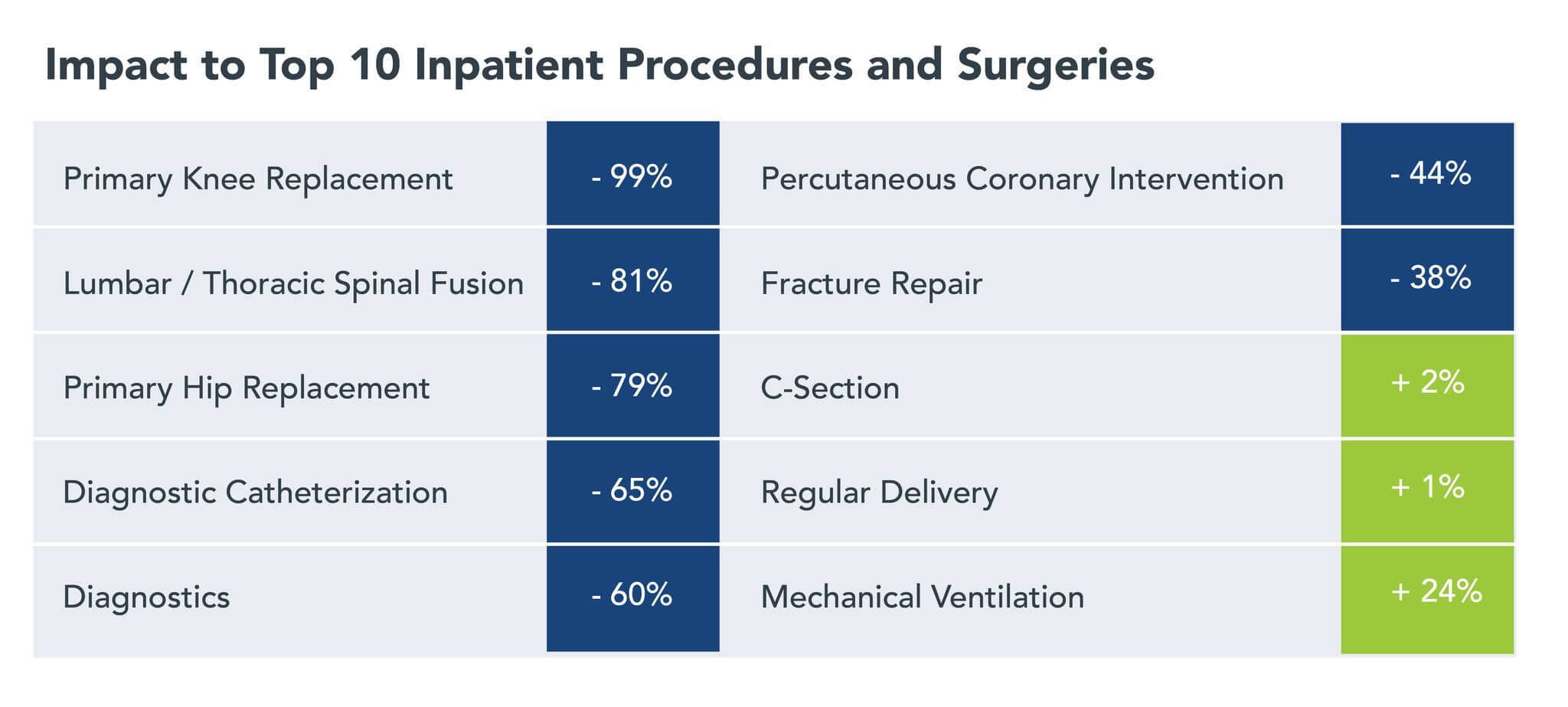
The chart from the Strata report depicts the volume activity in the top ten inpatient procedures. Babies kept coming and ventilator use skyrocketed to treat COVID-19 patients. Otherwise, volume plummeted.
Strata’s figures correspond with data from the Kaiser Family Foundation’s May tracking poll. KFF found that 48% of adults live in households where they or a family member have deferred necessary care during the coronavirus pandemic. Interestingly, only 11% believed that their medical conditioned had worsened without the additional care.
Given the steep volume declines and associated pent-up demand, Strata predicted in its May report that “millions of patients who put off care or had it delayed during the pandemic can soon be expected to flood hospitals and physician offices seeking care.” This was a reasonable prediction, but that patient surge never occurred.
With the exception of outpatient visits, volume has improved but not yet reached 2019 levels. Strata’s July 8, 2020 Tracker report found 30-day inpatient visits down 6.4%. Observation and emergency visits for the same period were down 15.1% and 22.4% respectively. There is significant regional and service line variation in these performance measures.
By contrast, outpatient visits were up 13.4% during the same period. As these contrasting inpatient and outpatient use patterns illustrate, consumers appear more comfortable receiving their care outside the hospital.
This creates a profound conundrum for hospital administrators: significant numbers of patients who require hospital care are not seeking it.
Embracing Humane Healthcare
Clearly, there are deeper experiential and behavioral forces reshaping demand for hospital services. Understanding and addressing these forces is essential to recapturing pre-COVID treatment volumes. Defining what constitutes humane healthcare is a good place to begin.
Environments are never neutral. They either heal or harm. Unfortunately, most healthcare spaces fall into the latter category. Their sterile character and antiseptic smell are unwelcoming, even intimidating. In short, they are not very humane. Patients fear receiving care in the best of times. COVID-19 has magnified their fears.
Healthcare organizations standardize service provision to improve outcomes and reduce costs. However, this relentless optimization leads to “one-size-fits-all” delivery mechanics that depersonalizes the experience of receiving healthcare treatments. Designed for catastrophic care delivery, physical treatment spaces are rigid and tone-deaf. At their worst, they become active impediments to healing.
While patient anxiety is not new to healthcare, the pandemic has amplified historic and systemic patient concerns regarding fear, inequality, and trauma in care delivery. Research into the emotional components of receiving healthcare services provides clues for both designing better healthcare spaces and re-engineering care delivery processes to accommodate individual patient needs during the different stages of their care journeys.
Gensler’s Pulse Survey identified the following characteristics that shape the experience of receiving healthcare treatments.
- Confidence Returns Through Relationships: While 35% of respondents have reduced confidence in the overall health system, only 4% have reduced confidence in medical professionals they know or consult with. 22% say it would scare them to consult with medical professionals they don’t know well.
- New Tools/Methods Can Be Unsettling: While 37% of respondents expect a digital pre-visit consultation at home, 28% say it would scare or confuse them. 30% would be confused by any additional paperwork/documentation that may be required for their digital consultations.
- Understanding Is Everything: 71% of respondents would like to fully understand their medical situation at their next doctor consultation. They consider dialogue with providers being the least stressful part of their journey experience.
- Personal Boundaries Can Be Deciding Factors: 44% of respondents would be scared or confused to agree to use new wearables for monitoring their health. 34% of respondents would be uncomfortable sharing basic health information with their employer.
- The Unknown Next Is Terrifying: 46% of respondents say realizing that they need a consultation itself is stressful. 45% find waiting for results stressful. 66% believe they are at their best when they know what’s happening next.
- Collective Health Is a New Paradigm: 60% of respondents desire to play a part in the health and wellness of the wider population, but 76% of them don’t know how or want easy ways to do so.
Understanding these behavioral characteristics is essential to configuring treatment venues with humane care delivery customized to individual consumer preferences. This is the essence of what is known as “platforming healthcare.”
Prototyping for Success
Most health systems lack the consumer instincts and retail sensibilities necessary to engage consumers. This lack of consumer sensitivity is a liability when seeking to restore consumer confidence. Without a clear understanding of the “pictures” inside consumers’ heads, it is difficult to address their fears, questions and apprehensions.
Retail companies excel at understanding consumer motivations and designing service solution to meet individual wants, needs and desires. Toward that end, they develop personas to match products and services to individual preference and proclivities. Gensler research has identified the following four critical characteristics (and eight behaviorally based prototypes) that shape the mindsets and expectations of healthcare users.
- Level of commitment (disengaged to engaged users)
- Ability to take action (hesitant to resolute users)
- Type of support needed (sensitive to pragmatic users)
- Awareness of the big picture (anxious to confident users)
The chart below places these behavioral dimensions on a spectrum with the resulting eight consumer prototypes.
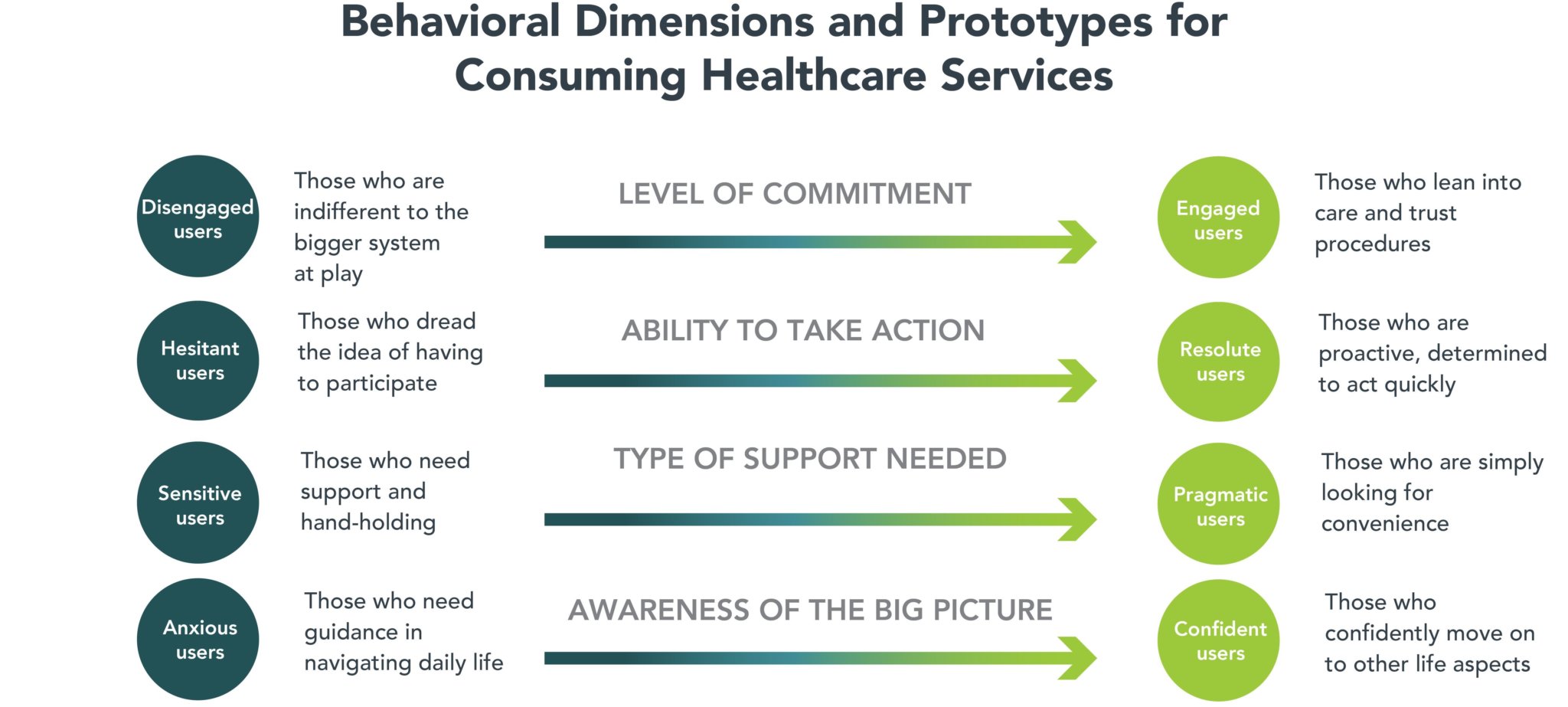
Identifying patient prototypes early and applying them throughout the care process enables providers to adjust both the practical and emotional components of treatment delivery. Done well, this type of personalized engagement creates a deeper level of connection between patients and caregivers. It enhances satisfaction, builds trust, and improves healing.
The coronavirus pandemic has exacerbated behavioral extremes. Race, geography, lifestyles, gender and socioeconomic status influence how individual consumers engage with providers. These characteristics make meaningful connection both more difficult and more important to achieve. Relationships with consumers take time and commitment to nurture and develop.
On the plus side, addressing COVID-related volume declines gives health systems the opportunity to develop their platforming and consumerism skills. This will not only help solve their short-term volume challenges; it will enhance their longer-term competitiveness.
Designing Post-COVID Care Delivery
Instead of designing physical and digital encounters and processes for one optimal solution, health systems can incorporate multiple, diverse ways of engaging consumers. Individualizing service in this way creates a sense of belonging, builds trust and promotes healing. It connects patients and providers organically. The best patient-provider relationships translate in intense brand loyalty and long-term engagement.
The following chart shows application of behavioral prototypes to the pre-visit, visit, and post-visit stages of a humane healthcare journey. The best healthcare experiences address patients’ emotional as well as their practical needs. Viewed from this perspective, a typical patient journey contains numerous opportunities for connection and engagement. These are the principal building blocks of establishing patient-provider relationship and — ultimately — brand loyalty.
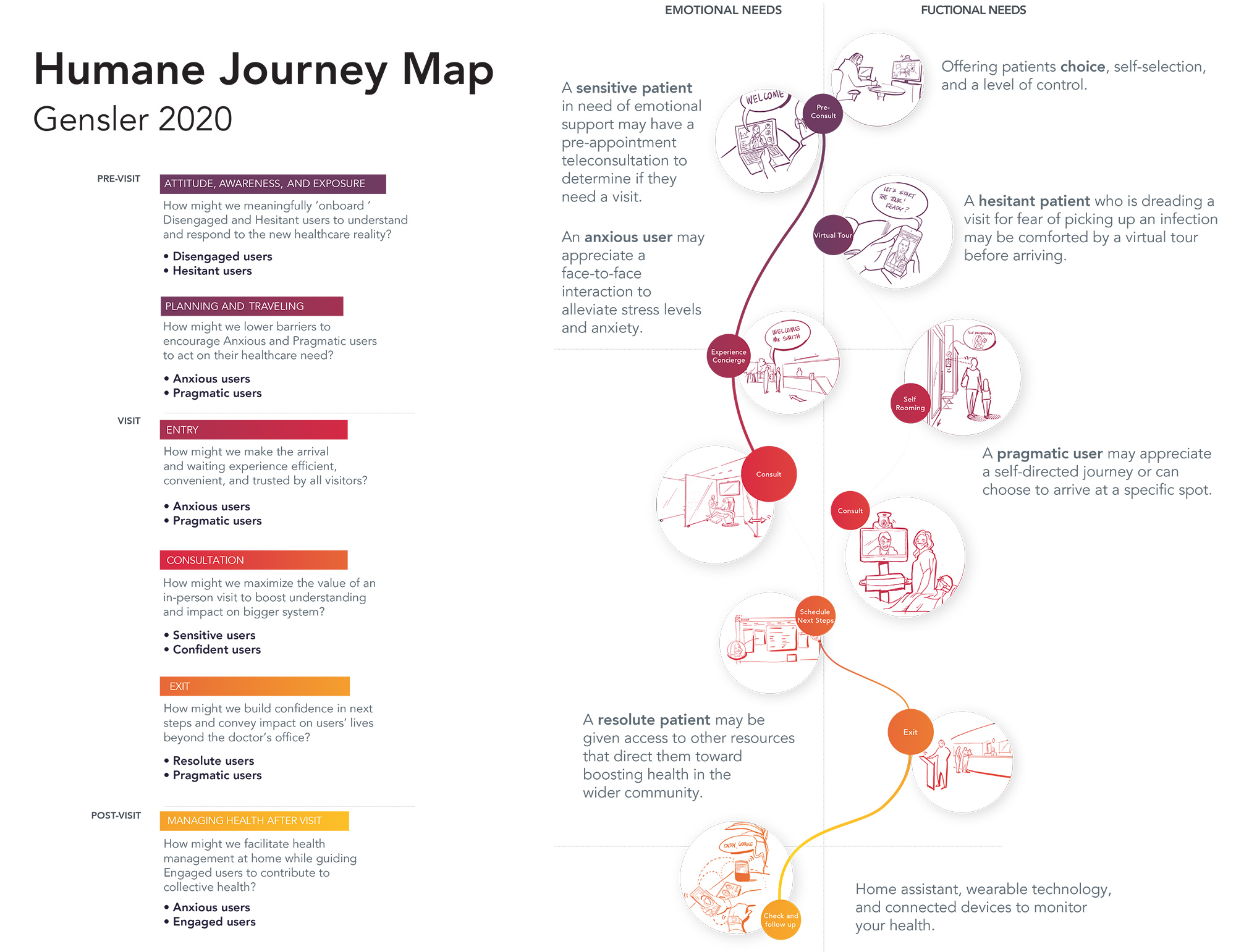
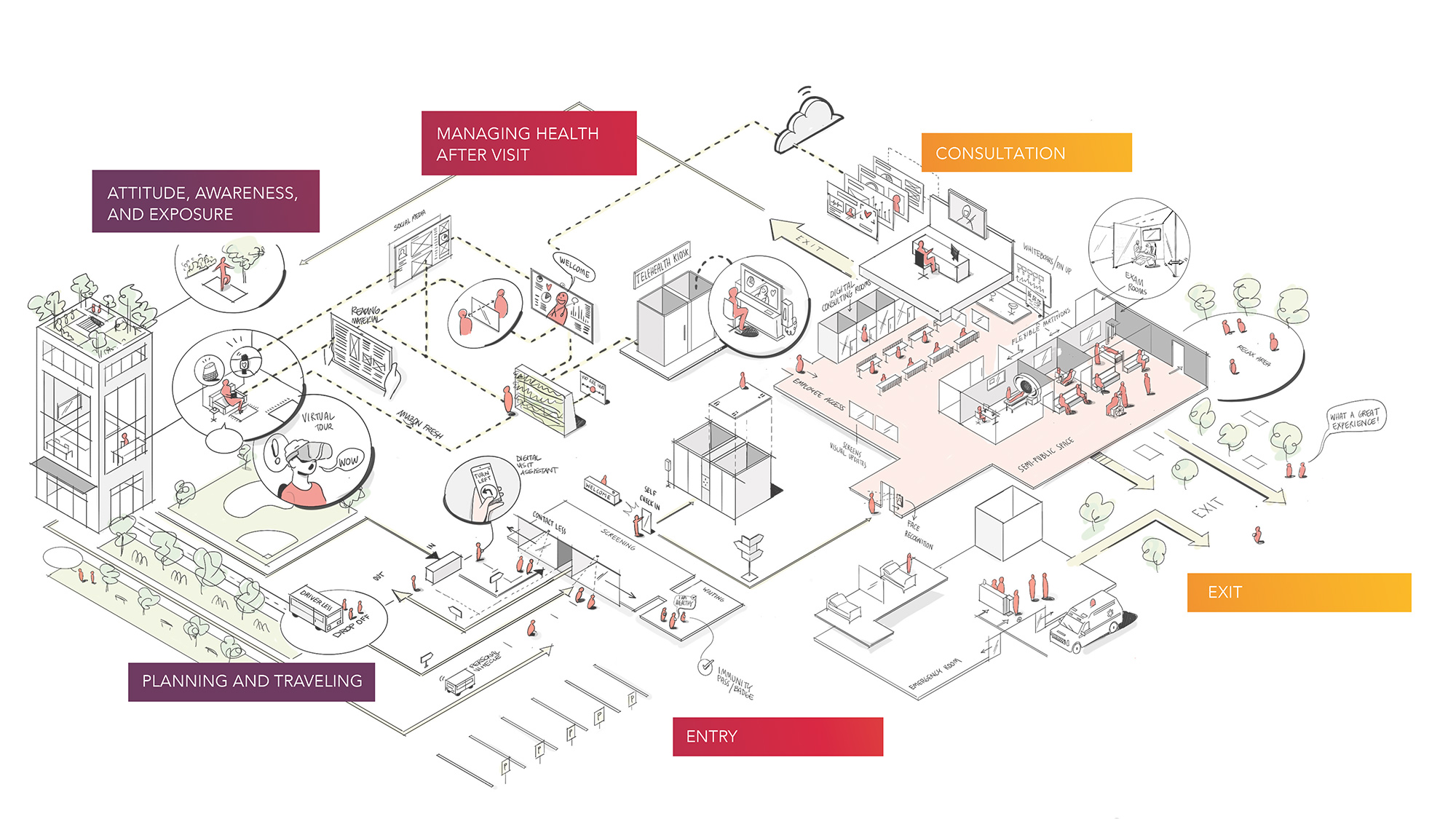
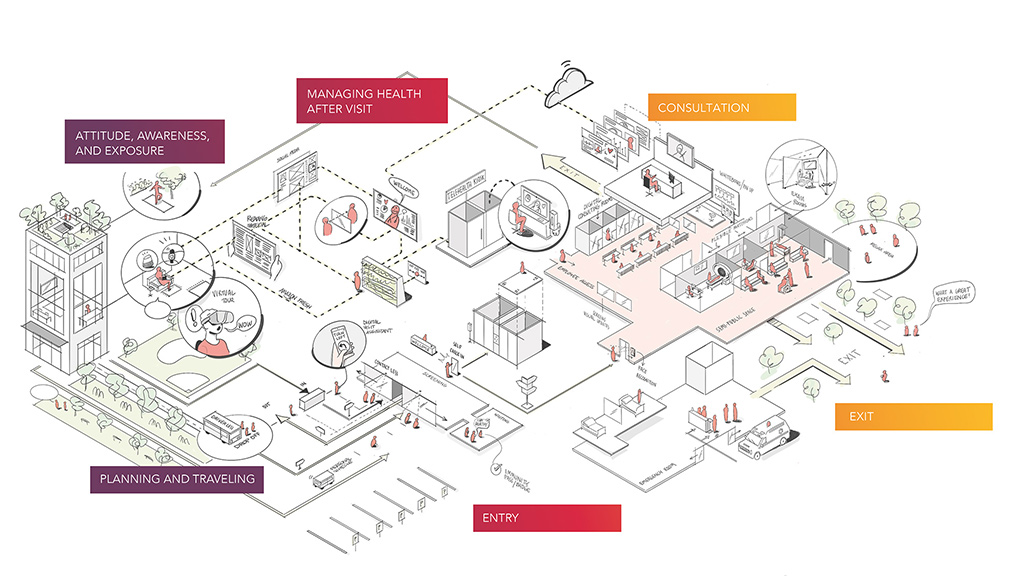
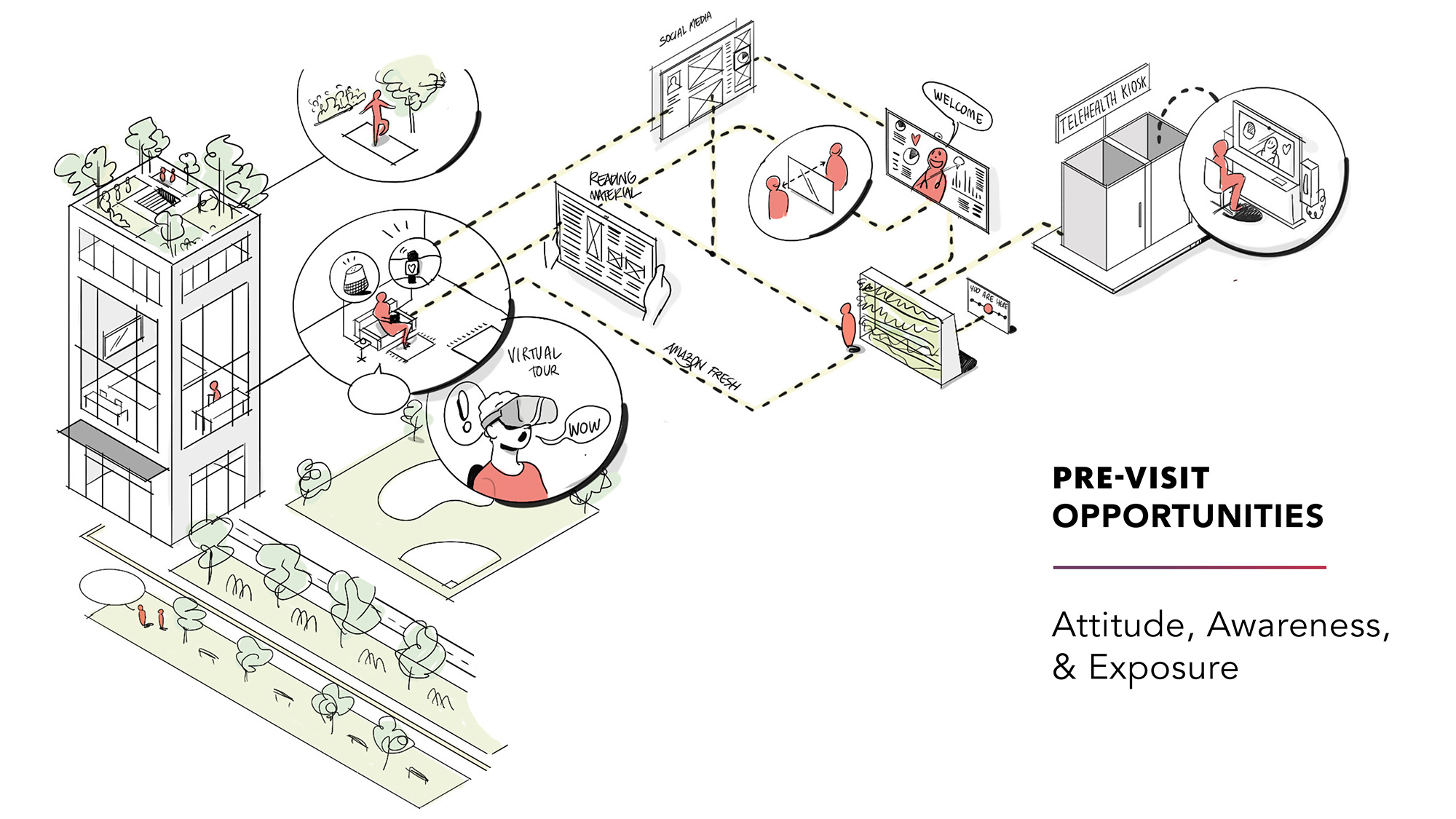
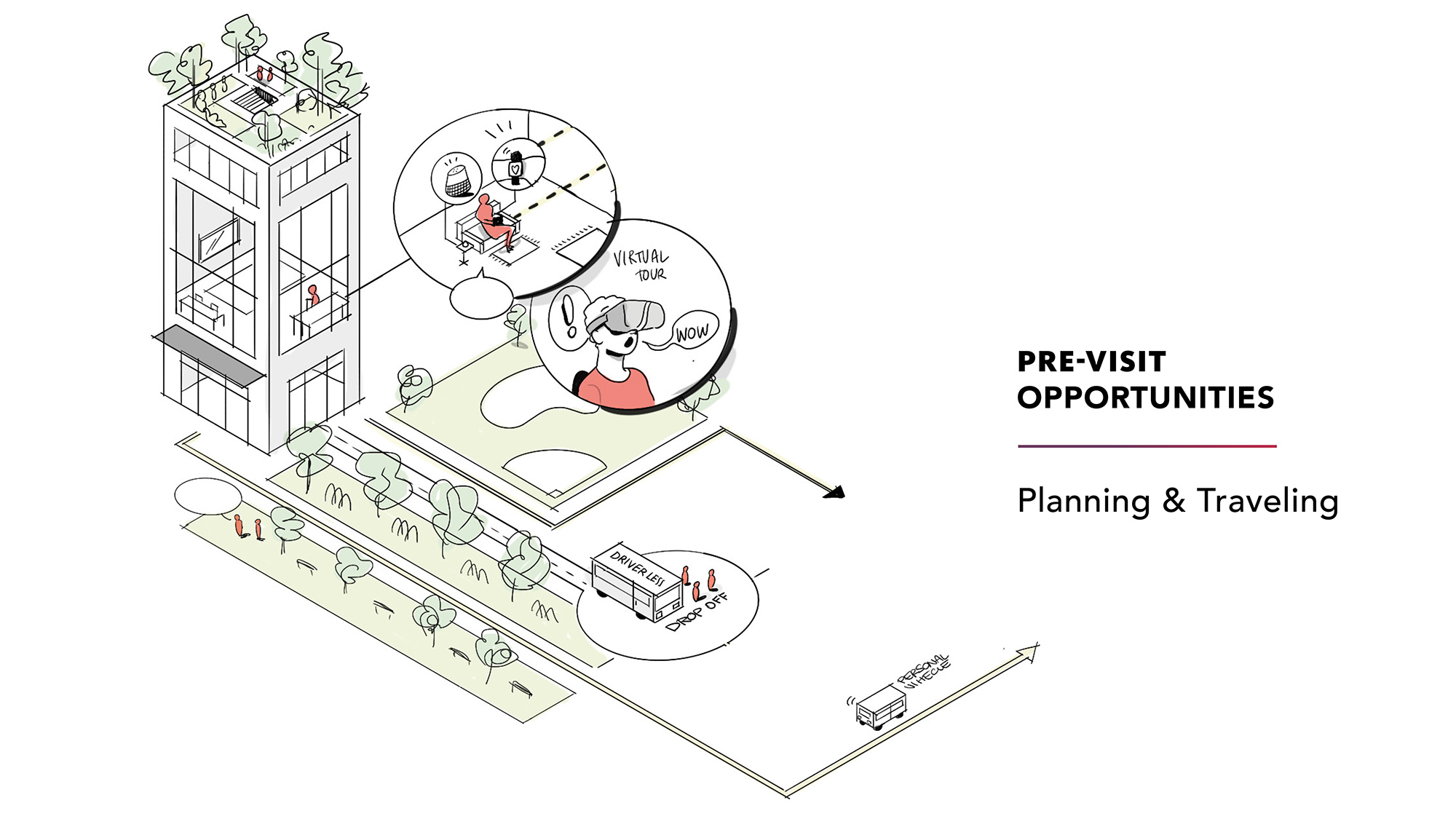
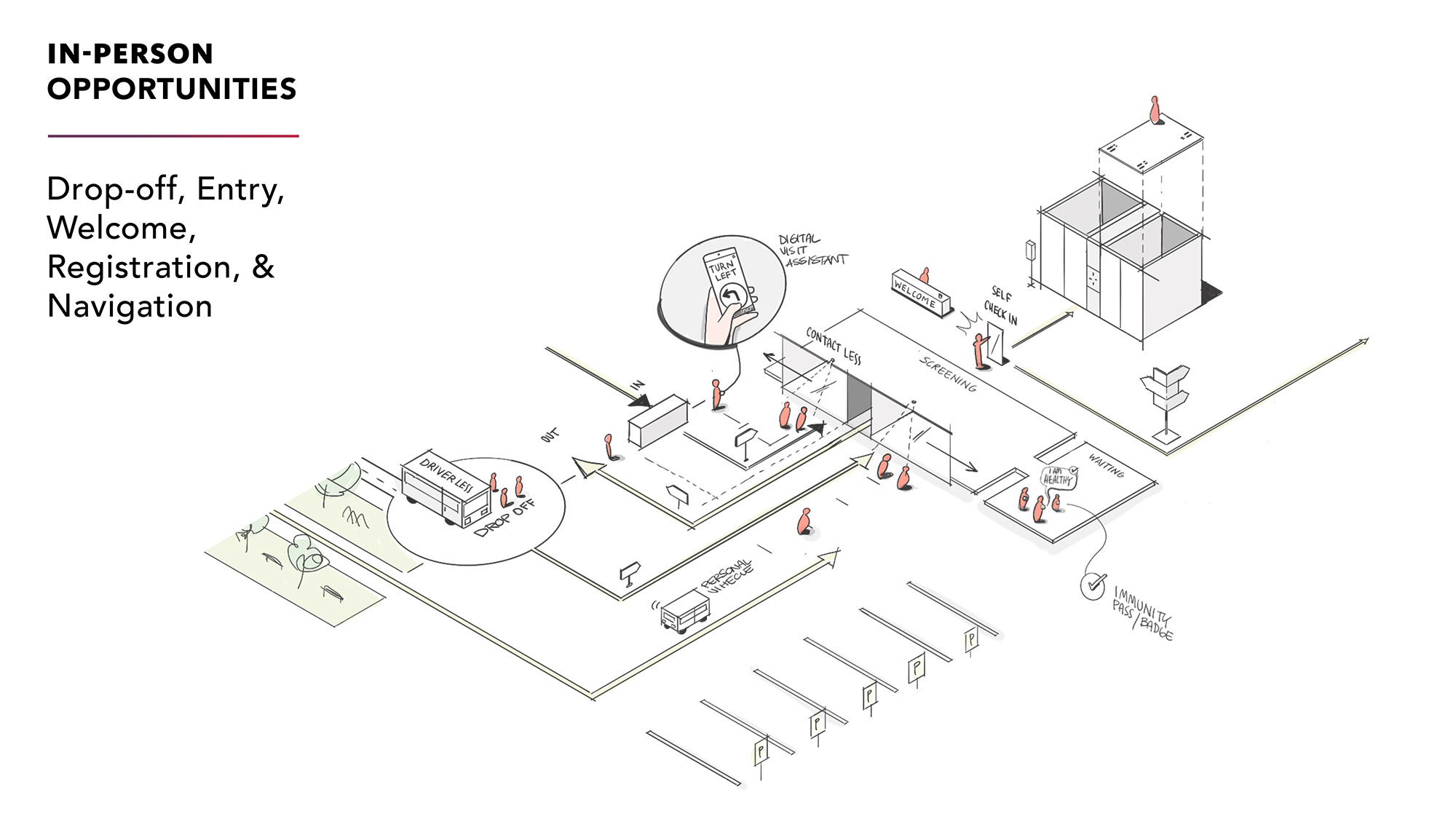
The following series of illustrations dive deeper into the pre-visit, visit and post-visit stages of the patient journey to explore opportunities to address the unique emotional and practical needs of prototypical users. In reviewing these opportunities, it is important to note that “digital space” is real space and integral to the seamless and holistic delivery of care.
Digital tools give the healthcare providers powerful new ways to engage patients and address their fears. Ultimately, care journeys transcend physical location and sequential care delivery. In this way, humane healthcare delivery addresses patients’ physical and emotional needs through personalized and integrated interactions that can be either virtual or physical. And in this way, humane healthcare offers the promise of customer experiences rivaling those offered by other consumer-oriented companies.
With rapid changes across the health landscape, connecting with users well before a medical need arises — whether through brand presence or involvement in other life aspects — helps in framing a productive state of mind. Disengaged and Hesitant users are in most need of our attention at this stage.
Sensitive and Pragmatic patients represent the two ends of user need at this stage: that of companionship and of convenience. Multiple modes of transport may need to be accommodated in this stage, with clarity and confidence in what’s next at each step.
Visibility of collective health is crucial at this stage. As all users — especially Hesitant and Pragmatic users — enter the facility, they need to see a confirmation of health. Once their mind is at ease, the focus will be on efficiency, convenience, and timeliness.
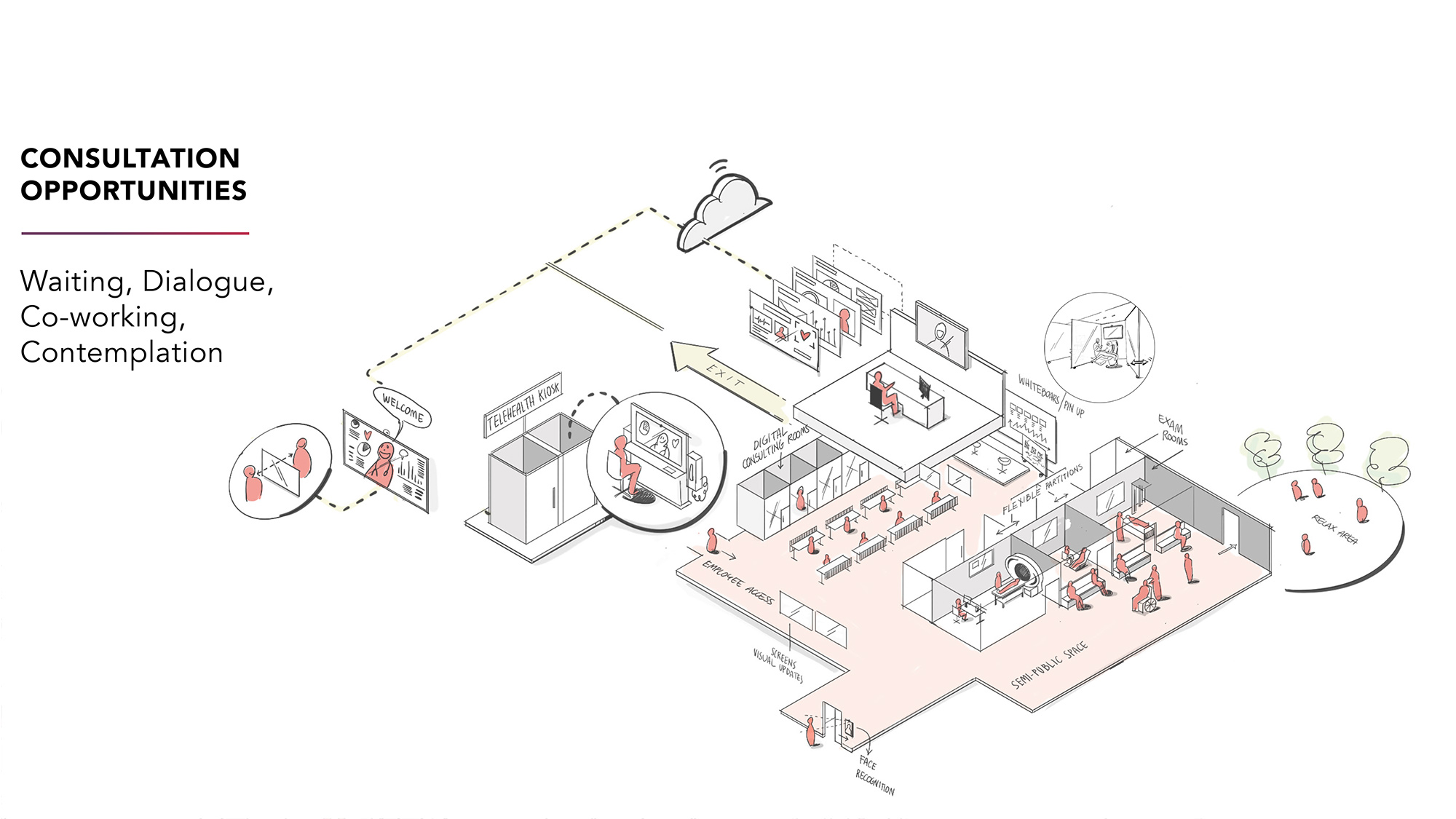
Humane healthcare is not just about the patients — but also the caregivers. Consultation is the stage that brings them in contact, with a new need to maximize time together. While Sensitive users may need reassurances, Confident users will need to grasp repercussions to daily life.
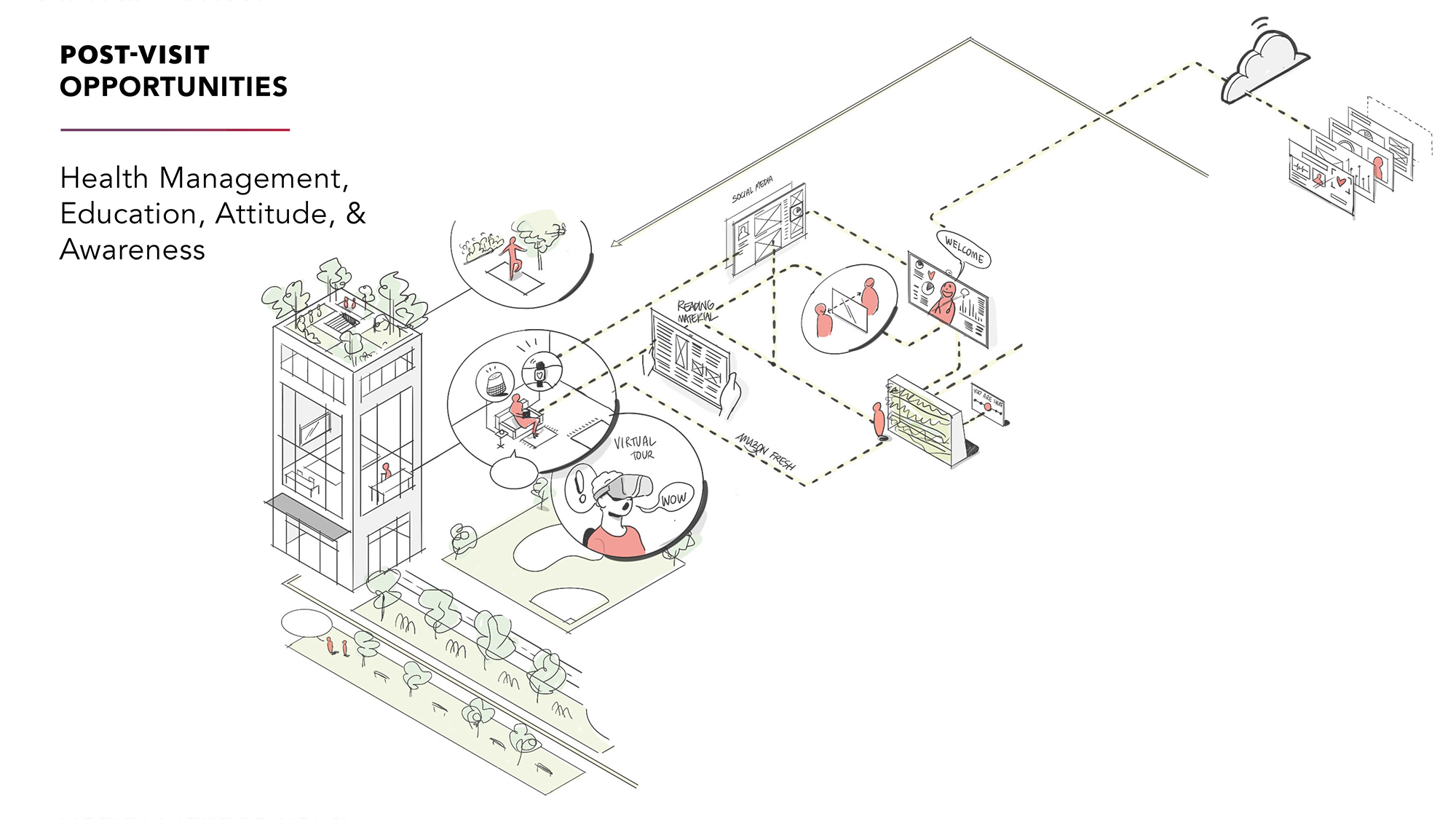
While Anxious users need guidance in navigating the new normal in life, Engaged users are looking beyond their individual health to contribute to collective health. New opportunities exist that can not only boost health at urban scale, but also spread the brand message.
Reimagining care delivery from patients’ perspectives outside the boundaries of pure architectural design opens new possibilities to improve outcomes, engage consumers, increase convenience, lower costs and build brand strength. These are the features that will distinguish winning health systems in the post-COVID marketplace.
Conclusion: Seize the Design
The coronavirus pandemic has created a global inflection point of a scale not seen since World War II. Historically, societies reorganize during these periods. Power relationships shift. Behaviors change. Markets adapt. Industries rise and fall.
The pandemic’s disruption of traditional delivery mechanics creates opportunities for health systems to rethink and modify traditional business practices and behaviors. The remarkable increase in virtual care delivery testifies to providers’ collective ability to embrace change, overcome obstacles and meet patient needs under duress.
In this sense, health systems have the once-in-a-generation opportunity to reinvent themselves as consumer-directed platform companies. As they work to regain consumer trust amid the coronavirus pandemic, health systems can create the foundation for more humane, integrated and successful business models.
Employing forward-looking crisis management during the pandemic will enhance longer-term organizational repositioning. Facility and process redesign are essential to addressing the short-term operational challenges posed by COVID-19 and realizing the longer-term benefits of strategic repositioning.
It is not a coincidence that brand guru Alina Wheeler noted that “Design is intelligence made visible.” The effort required to understand and respond to consumers’ healthcare needs will manifest itself in greater customer engagement and stronger brand loyalty. Design is the primary mechanism through which companies respond to consumers, build their brands and sustain competitive advantage.
Consumer engagement has been healthcare’s biggest challenge as the industry transitions to value-based care delivery. Properly understood, engaging customers can be the most effective strategy for health systems to increase their market relevance.
German typographer Oti Aicher believed that “Good art inspires and good design motivates.” Aicher’s pictograms for the 1972 Munich Olympics inspired new forms of public signage that enable people speaking multiple languages to navigate urban environments. Using good design to motivate better healthcare services is “intelligence made visible.”
Carpe diem is Latin for “seize the day.” Carpe design is the formula through which health systems care create humane healthcare throughout multiple environments that delights customers, inspires caregivers and delivers superior outcomes without breaking the bank.
For media inquiries, email .