Test, Don’t Guess: A New Approach for Healthcare Design
Healthcare leaders are modeling multiple futures before breaking ground — shifting from fixed bets to flexible strategies.

For decades, healthcare facility planning meant investing millions in a single “best” design and hoping it worked. But what happens when your best guess is wrong?
Today’s reality is sobering: inpatient stays have dropped 19% while outpatient visits have surged 31%. Facilities built for yesterday’s care models now struggle with capacity bottlenecks and staffing shortfalls, as budgets shrink and patient needs evolve. The old guess-and-build approach looks increasingly like an expensive gamble.
A growing number of healthcare organizations are refusing to guess. They’re testing three, four, even five different care models in the same footprint before breaking ground — comparing everything from nursing station layouts to staffing patterns, understanding real costs and workflows before committing a single construction dollar.
This isn’t just a new planning method. It’s a fundamental shift in thinking about healthcare space: from fixed bets on one future to strategic investments tested against different future scenarios.
What’s Driving the Space Revolution?
The convergence of financial pressures and evolving care models has created an inflection point for healthcare facilities. Organizations that once expanded footprints to accommodate growth now face a different challenge: making existing spaces work harder and smarter while improving patient outcomes.
We’ve found that healthcare leaders are asking fundamentally different questions. Instead of “How much space do we need?” they’re asking, “How can our current footprint better support our evolving care delivery model and enhance the patient experience?” This shift signals a transformation in how healthcare organizations view their physical assets — not just as cost centers, but as critical enablers of quality care.
What’s Working — and What to Avoid
After analyzing dozens of healthcare facility optimization projects, four clear patterns emerge among organizations that successfully transform their spaces. These approaches not only drive better outcomes — they also help avoid the most common planning pitfalls:
What’s Working?
The Power of Data-Informed Design
Making Data-Informed Decisions: Using simulation tools prevents over-specialization and quantifies operational metrics and patient impact before construction begins.
Modeling Multiple Scenarios: Testing various care delivery models within the same footprint enables an assessment of operational and care implications to inform the best fit for each organization.
Testing Movement Patterns: Prioritizing flow analysis over static layouts reveals hidden inefficiencies and prevents costly workflow disruptions before they’re built.
Including Human Factors: Incorporating organizational readiness into planning simulations helps identify and address cultural barriers. Without buy-in and training, new workflows may fail to take hold, wiping out projected efficiency gains.
What to Avoid?
Common Pitfalls in Healthcare Planning
Over-Specializing Space: Creating highly specialized procedure rooms leads to costly underutilization — with rooms sitting idle 50% of the time, while general examination spaces remain overbooked and patients wait longer.
Planning for Outdated Models: Facilities planned for traditional inpatient care struggle to adapt to ambulatory-focused models, while those designed around physician-centric care face challenges in implementing team-based approaches.
Ignoring Workflow Reality: Floor plans often don’t capture operational complexity. One medical center placed supply rooms at the building ends to maximize patient space — resulting in thousands of extra staff steps per shift, doubled restocking times, and increased turnover.
Underestimating Cultural Readiness: Moving from physician-centric to team-based care requires more than reconfigured walls — it demands new workflows, extensive training, and often challenges existing departmental hierarchies.
Advanced simulation platforms exemplify this approach in action. Teams can quantify the impact of different operational models, discovering, for instance, that distributed nursing stations reduce staff walking distance by 40% — freeing up an estimated 90 minutes per nurse per shift for direct patient care.
These tools reveal how patient flow patterns change between traditional and team-based care models, visualizing bottlenecks that create not just operational inefficiency but patient stress and confusion. Most critically, simulation technology allows organizations to test five, even 10 different scenarios — from fixed room assignments to fully flexible units — comparing hard metrics on utilization, staff efficiency, operational costs, and projected patient satisfaction scores before committing millions to construction.
Case Study: Enloe Health’s Strategic Approach
The recent consolidation of multiple cardiology practices into Enloe Health’s new cardiovascular clinic illustrates contemporary best practices in facility planning. Rather than simply scaling up existing layouts, the design team explored multiple care delivery models to understand how each would impact operational performance and space utilization.
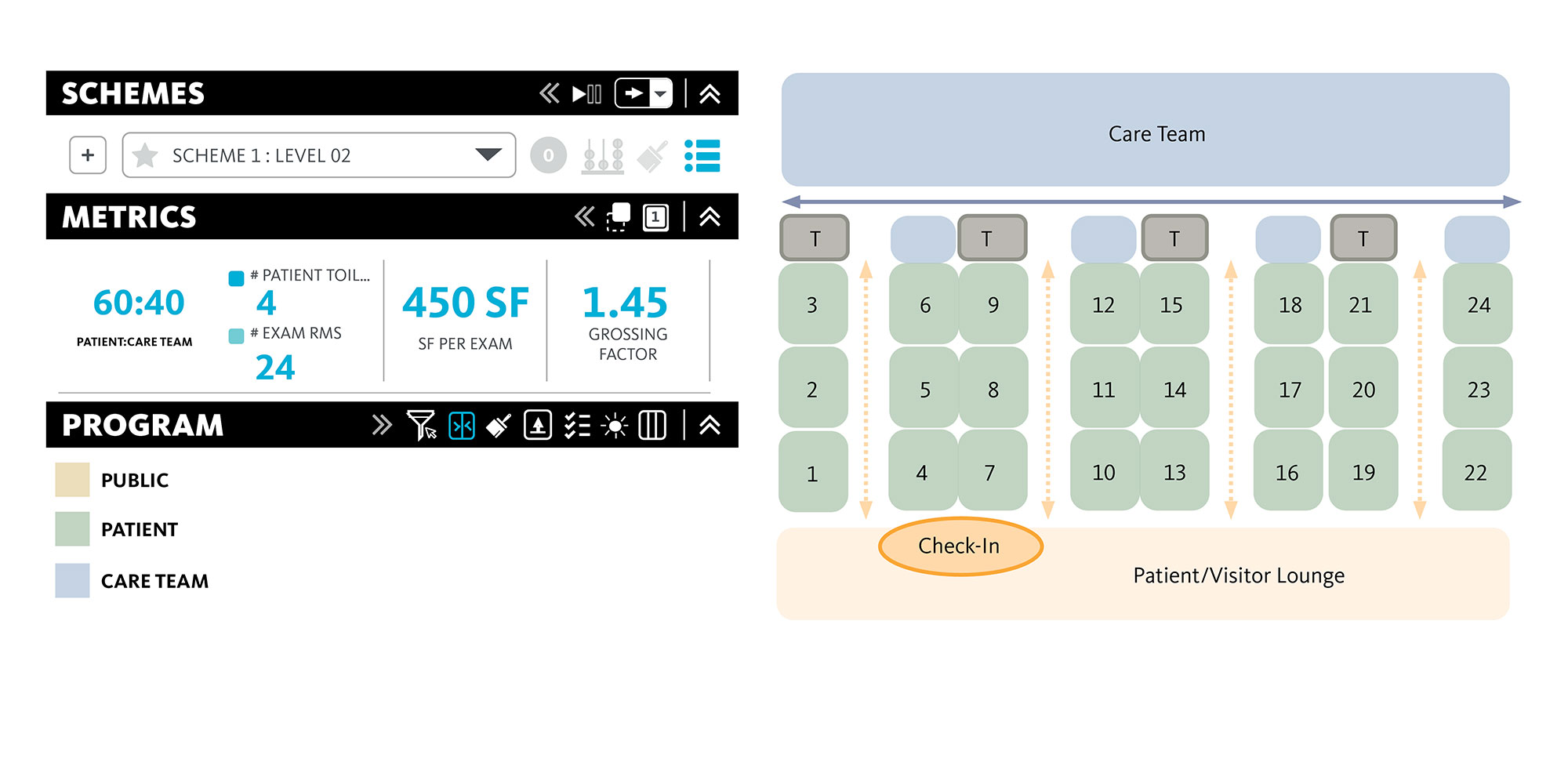
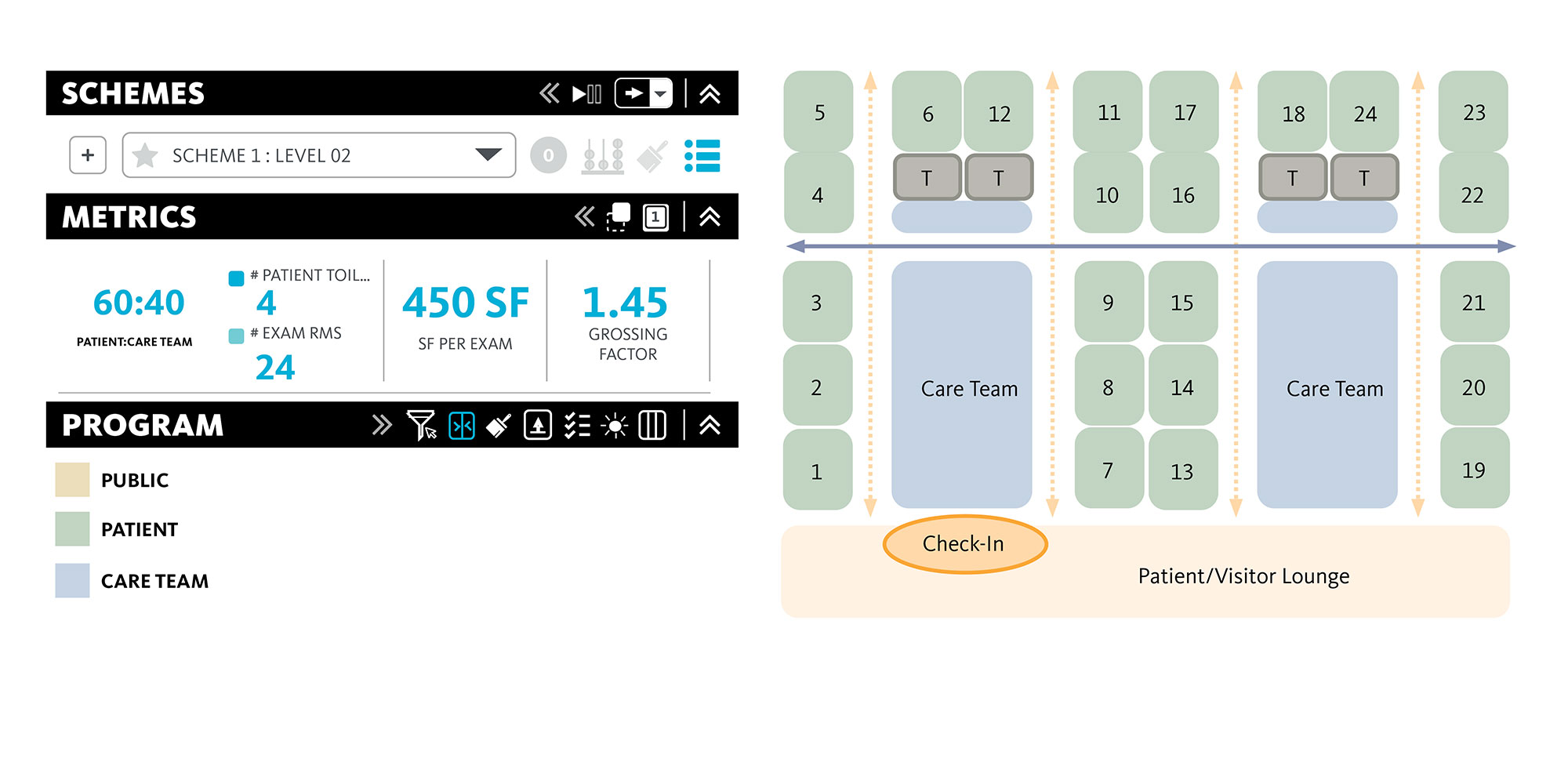
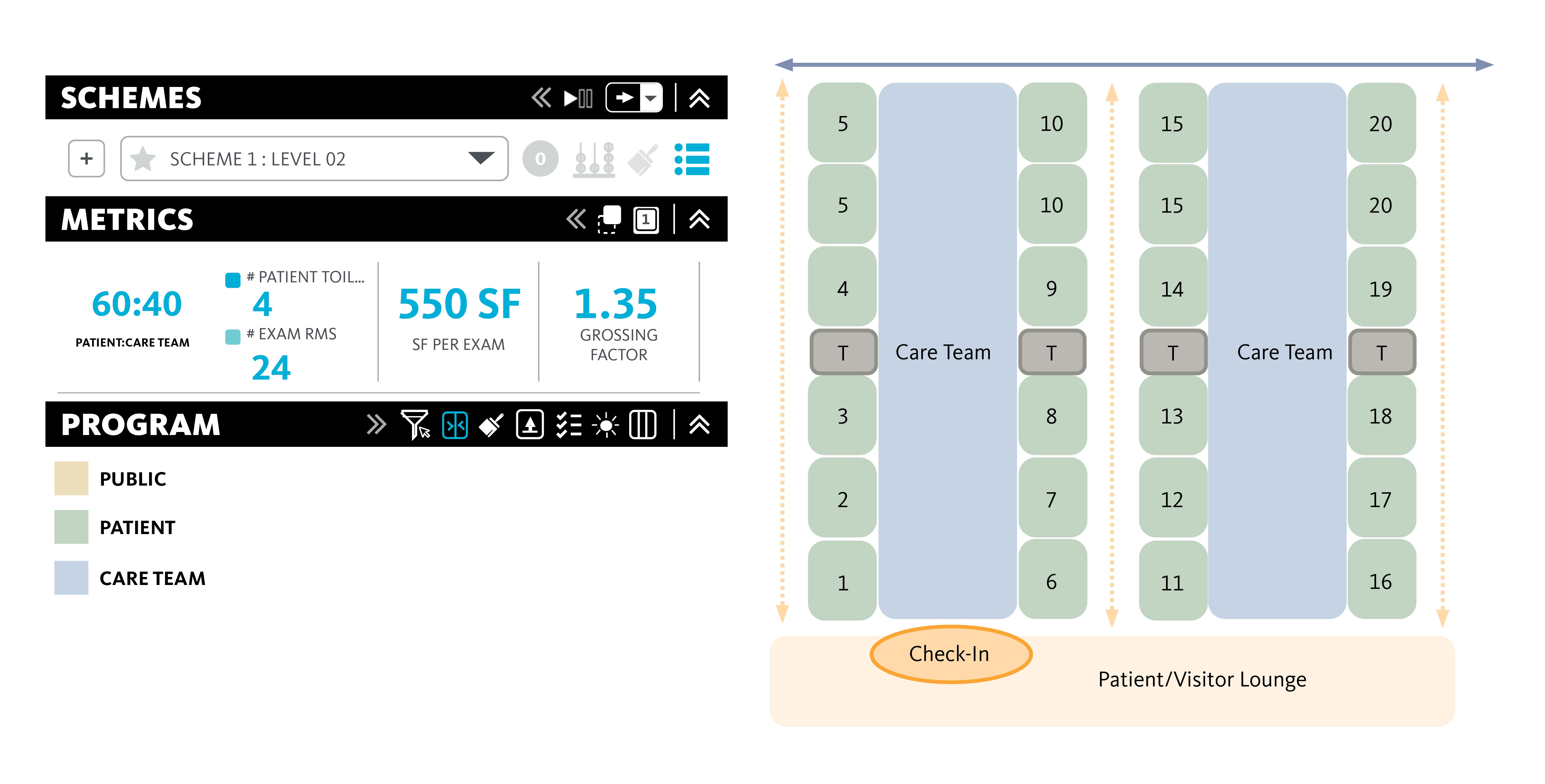
The team developed and tested three distinct care delivery models, each differently affecting space utilization, staffing patterns, and patient flow. Using gFloorz, Gensler’s proprietary simulation tool, they could visualize and quantify the operational and efficiency impact of each model before making design decisions.
Through this data-driven design process, gFloorz revealed critical insights:
- Patient navigation efficiency varied significantly between care models, with some offering more streamlined and efficient circulation patterns, and others with higher space efficiency ratios and public waiting areas.
- Room utilization varied by up to 30% between models; one model allocated more space to treatment and care team spaces by reducing private provider office workspace.
- Staff travel distances differed by nearly half a mile per day, depending on configuration.
This simulation process helped Enloe select a model that aligned with both clinical goals and financial sustainability — ensuring the new facility would be agile, efficient, and future-ready.

Three Truths from a Decade of Transformation
Having witnessed hundreds of facility planning projects, from minor renovations to major new constructions, certain truths have become evident:
Space optimization isn’t about making do with less — it’s about aligning physical resources with organizational strategy. The most successful projects start with a deep understanding of care delivery goals.
Technology tools are enablers, not solutions. The value doesn’t come from the simulation software itself, but the questions it allows teams to ask and answer. The best outcomes emerge when technology supports the planning process, rather than driving it.
Finally, the most important lesson may be that perfect optimization is less valuable than continuous adaptation. Healthcare facilities that can evolve with changing needs will outperform those optimized for a single point in time.
Today’s most successful healthcare organizations aren’t necessarily the ones with the newest or largest facilities, but those that align their space with their mission and their patients’ needs — and adapt continuously. In an industry where every dollar matters, every square foot has cost implications, and every design decision impacts patient care, agility is now a strategic imperative.
For media inquiries, email .