dialogue BLOG
Personal insights and opinions from Gensler’s global experts on how design is shaping the future of cities. Subscribe to our dialogue Now newsletter to get regular updates sent directly to your inbox.
1074 Items

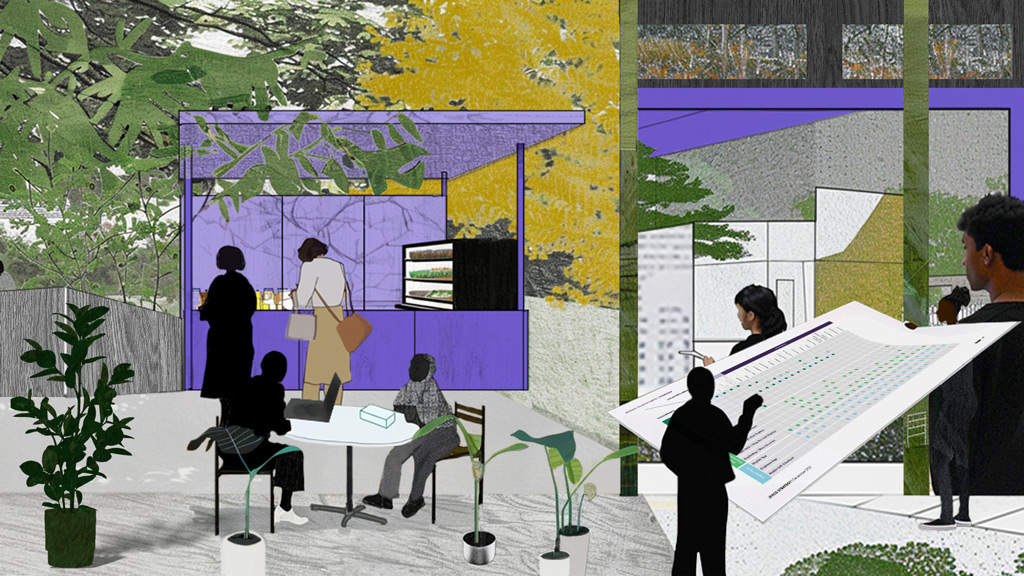
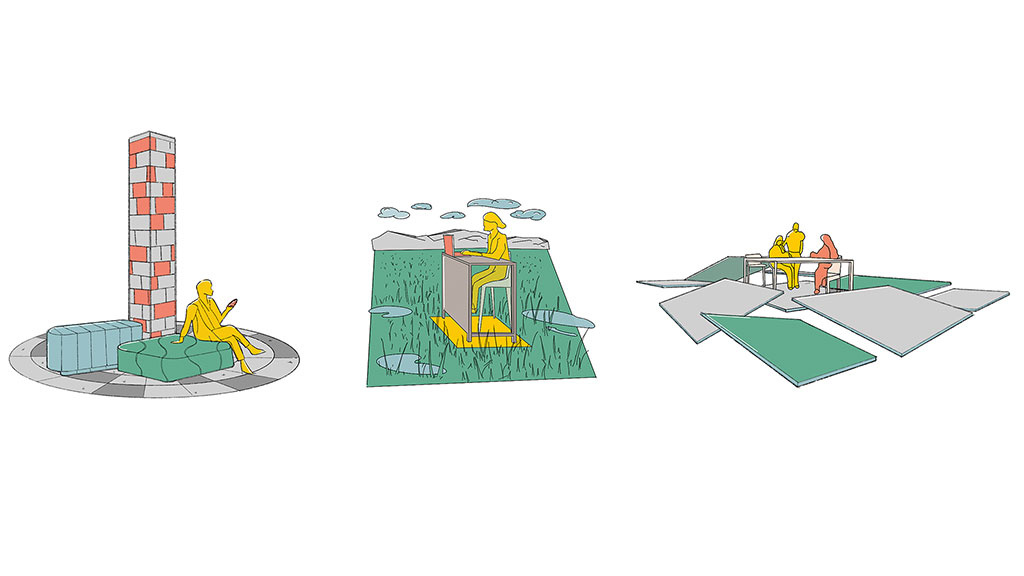
Beyond Blueprints: What Happens When Students Redesign Cities
The urban planners and architects of today and tomorrow must offer strategies that tackle complex, cross-cutting urban challenges with creativity.
December 19, 2025
|

Seattle’s Office-to-Residential Future: How Policy and Design Will Transform Downtown
A combination of code changes, design expertise, and market conditions is proving that now is the time to start planning new housing in Downtown Seattle.
December 16, 2025
|

Trends to Watch: What’s Next for Airports and Aviation
Gensler’s Aviation leaders take a closer look at the trends shaping the future of travel, and what’s next for the industry.
December 09, 2025
|

Trends to Watch Shaping the Future of Sports
Gensler’s Sports leaders explore the design trends redefining the next era of sports design, from fan-first districts to athlete-driven spaces.
December 09, 2025
|

10 Workplace Trends for 2026: What’s In and What’s Out?
This is the year of bold moves, human-first thinking, and AI that doesn’t just answer questions but joins the team.
December 05, 2025
|

How Design Can Advance Diverse Nonprofit Missions
Nonprofits can use architecture and design strategies in campus development to amplify their mission impact and operational excellence
December 03, 2025
|

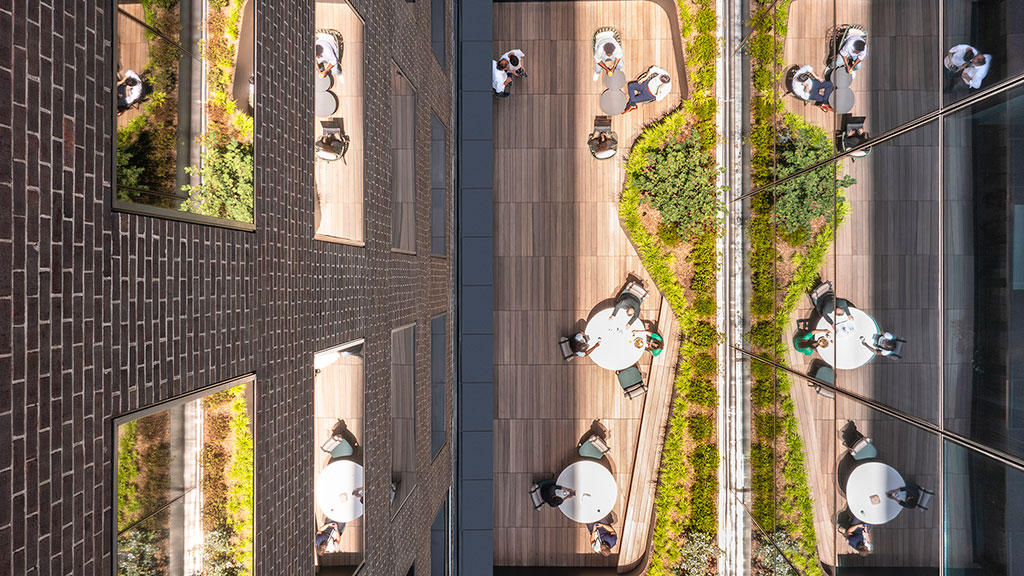
How Nokia’s New R&D Campus Raises the Bar for Canada’s Tech Ecosystem
The company’s new space in Ottawa replaces the traditional workplace model with one centered on employee experience.
December 02, 2025
|

Trends to Watch: How Global Events Build Magnetic Place Brands
From the Super Bowl to the FIFA World Cup, marquee events transform urban environments into platforms that amplify civic pride and create lasting impact.
November 24, 2025
|

Transforming Pier 94: A Collaborative Journey in Sustainable Design and Adaptive Reuse
Pier 94 on Manhattan’s Hudson River waterfront will soon be home to New York City’s first purpose-built, state-of-the-art film and television production facility: Sunset Pier 94 Studios.
November 21, 2025
|

Designing the Future of Travel at Pittsburgh International Airport
Building a terminal rooted in flexibility, passenger experience, and the spirit of a city that’s reinventing itself.
November 19, 2025
|

NEXT NEXT: Redefining Science Work for the AI and Machine Era
Our new concept looks at how AI and automation are redefining the science workplace and reshaping the future of labs.
November 18, 2025
|

Test, Don’t Guess: A New Approach for Healthcare Design
Healthcare leaders are modeling multiple futures before breaking ground — shifting from fixed bets to flexible strategies.
November 14, 2025
|

Inside Bangalore’s Talent Race: The Power of Purposeful Workplace Design
While Bangalore continues to face real challenges, such as aging infrastructure, relentless traffic, and a growing water crisis, the city is emerging as a strategic hub for global workplace expansion and a magnet for newcomers.
November 14, 2025
|

The New Job for the Airport CEO: It’s More Challenging — and More Uplifting — Than Ever
In this pivotal moment, we have an opportunity to design airports and terminals that feel less like infrastructure and more like inspirational destinations.
November 12, 2025
|

Designing Tomorrow’s Shopping Centers: Global Ideas From Kuwait, Costa Rica, and Beyond
Around the world, developers are experimenting with new models that expand the meaning of “retail.” For U.S. retail designers, these examples offer valuable lessons for an era defined by shifting consumer behavior, climate pressures, and the need to create authentic community experiences.
November 12, 2025
|

Beyond the Screen: Making Digital Beauty Brands Shine in Real Life
How digital-first retailers can navigate the crucial transition of a brand into physical space.
November 12, 2025
|

Reinventing the Strip: How to Make Everyday Retail Irresistible
What makes a strip mall “successful”? Discover the formula for staying local, lively, and loved.
November 12, 2025
|

How Journey Mapping Shapes Design Opportunities for the User
Journey mapping is more than a tool. It helps teams visualize how users move through systems, spaces, and services over time, capturing not just what users do, but how they feel, what they expect, and where they encounter friction or delight.
November 12, 2025
|

More Than Just a Seat: The Lounge as the New Travel Destination
The new airport lounge is less about claiming a seat and more about creating a collection of experiences.
November 04, 2025
|

A New Hybrid Hotel Blends Japanese Culture and Texas Charm
The Miyako Hybrid hotel rethinks hospitality through a Texas-Japanese fusion hotel experience.
October 27, 2025
|

The New Economics of Sports Venue Design
From NIL-driven college athletics to multi-tiered VIP lounges and mixed-use districts, sports venues are evolving into dynamic business ecosystems.
October 22, 2025
|

How a New Vision for Flexible Co-Living Conversions Can Support Housing Affordability
Gensler and The Pew Charitable Trusts studied building typologies in 10 cities to better understand the potential in this unique office-to-residential conversion model.
October 21, 2025
|

San Francisco’s AI Boom Is Our Chance to Build a People-First City
The AI gold rush presents a rare opportunity to reinvest in our urban core, reconnect our neighborhoods, and rebuild our streets.
October 14, 2025
|

Age-Welcoming Cities: Designing for an Era of Longevity
The challenge of a rapidly aging population also presents an opportunity: to reimagine how we plan our cities.
October 14, 2025
|

Mixed-Use Developments: A Sustainable Blueprint for Urban Growth
High-density mixed-use developments can be a powerful engine for economic growth, resilience, and cultural and socioeconomic cohesion.
October 14, 2025
|

A Multigenerational Workforce Demands Multigenerational Design
Employees over 65 are defying stereotypes and redefining expectations. Organizations that design with them in mind won’t just gain an edge today — they’ll shape the future of work.
October 08, 2025
|

The Future of Real Estate Metrics: Human Connection
The places that thrive in the years ahead will be designed to build relationships, inspire belonging, and foster togetherness.
October 07, 2025
|

Birmingham Living: The Next Chapter
This Q&A with Gensler residential leaders John Badman (London) and Jamie Rodgers (Birmingham) explores how Birmingham’s evolving housing market is shaping the city’s next chapter.
October 06, 2025
|

Where Champions Train
For the WNBA’s Phoenix Mercury and the Las Vegas Aces, world-class training and practice facilities helped propel them to the top of their game — and the league.
October 03, 2025
|

How Aviation Is Evolving for the Leisure Traveler
Airports are in the midst of a profound transformation. Confronted with aging infrastructure, rapidly advancing technology, and an unprecedented surge in leisure travel, these once utilitarian spaces are being reimagined as destinations in their own right.
October 01, 2025
|

Reimagining San Diego International Airport’s T1 as a Global Gateway
A bright, new modern terminal and roadways transform the travel experience.
October 01, 2025
|

Designing a 24/7 Entertainment Hub in Reno
The Grand Sierra Resort Reno Arena is more than a sports venue; it’s a fully integrated destination built around seamless entertainment.
September 30, 2025
|

Designing German Cities and Workplaces for a Thriving Economy
Gensler Germany’s leaders explore how urban design, workplace innovation, and strategic investment in public and private spaces can strengthen German cities.
September 29, 2025
|

Scaling Circular Design: Key Policies, Standards, and Strategies
As momentum grows for circular design, cities and clients face significant challenges and opportunities to implement it widely.
September 24, 2025
|

Climate Change Is Threatening What We Love About Cities
If cities hope to thrive in the face of climate change, they’ll need to balance emotional connection with environmental resilience.
September 23, 2025
|

The Carbon Impact of a Workday
When people calculate their carbon impact, they typically consider their cars, food, clothes, and flights. But they rarely consider where they spend their day. It’s time to change that.
September 22, 2025
|

Designing a New Way to Think in the Age of AI
Gensler co-CEO Jordan Goldstein speaks with Kristen Conry, Senior Vice President of Global Design, Marriott, about how AI is blending creativity with operations, storytelling with strategy, and vision with impact.
September 19, 2025
|

7 Myths Dogging Efforts to Fully Electrify Buildings — Let’s Bust Them
Despite misconceptions, building electrification is a practical and beneficial choice for many building owners.
September 19, 2025
|

Human and ‘Digital Employee’ Collaboration Will Transform Workplace Design
AI integration will soon impact physical spaces, potentially reshaping individual and group culture within organizations.
September 17, 2025
|

Reimagining Haussmann: Adaptive Workplace Design in the Parisian Urban Fabric
A look at how we can adapt these historic apartments to become sustainable, flexible, and human-centered workplaces for the future.
September 17, 2025
|

Retrofit at Scale: A New Blueprint for Investible Urban Development
A conversation with Gensler’s Harry Cliffe-Roberts and Opportunity London’s Jace Tyrrell on why retrofit is emerging as a preferred solution — and how this cross-industry guide is helping move the dial.
September 16, 2025
|

Design as Storytelling: How AI Is Transforming the Way We Imagine, Create, and Connect
AI isn’t here to replace creativity. It’s here to amplify it — helping us move from inspiration to iteration with greater speed and substance.
September 11, 2025
|

Energy Meets Art: How Museums Are Rethinking Climate Control
Energy-saving regulations and new techniques are prompting museums to reexamine how they manage indoor climate control.
September 11, 2025
|

How San Francisco Can Apply Startup Culture to Unlock Housing Solutions
We explore four strategies to bring iterative, bold approaches to address the city’s housing shortage.
September 10, 2025
|

Why Japan’s Workplace Trends Are Moving Against the Global Current
How companies in Japan can adapt their workplace solutions to counteract the country’s stagnating office experience.
August 27, 2025
|

Six Decades of Creativity: Interior Design Magazine Celebrates Gensler’s 60th Anniversary
The industry publication marks a milestone in the firm’s history with a roundup of global projects and people shaping what’s next in design.
August 25, 2025

Why Modern Hiring Centers Matter in Today’s Competitive Job Market
With thoughtful, strategic design, a hiring center or interview suite can be a valuable asset to attract top talent.
August 22, 2025
|

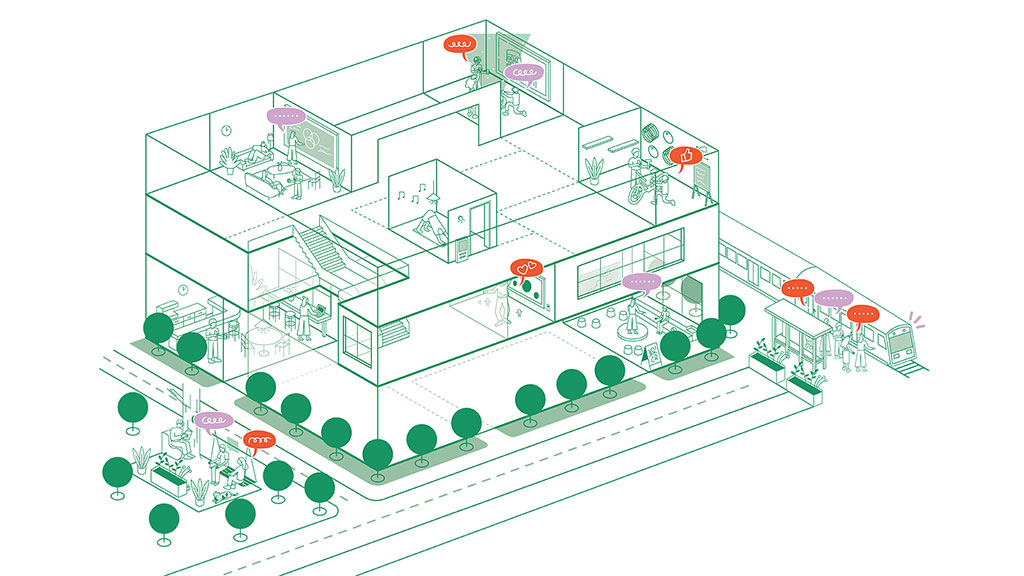
Designing Workplaces That Work — With Your People
When employees are involved in the planning and design process, the workspaces we create are more effective, engaging, and human.
August 21, 2025
|

Blueprint for Change: How Modern Training Centers Are Redefining the Trades
With thoughtful design, modern training centers for skilled trades are reshaping perceptions of vocational education.
August 18, 2025
|

How Business Schools Are Embracing Workforce Preparedness and Student Well-Being
To prepare students for success, campuses are becoming interdisciplinary, flexible environments that foster career readiness and holistic growth.
August 18, 2025
|

Trends to Watch Shaping the Future of Student Housing
In a time of great market uncertainty, student housing is proving to be a good investment for developers and revenue-positive for campuses.
August 13, 2025
|

Designing Campus Spaces for Tomorrow’s Workers in the Age of AI
Higher education institutions that embed human-plus-technical skills into an ecosystem of third spaces will help prepare tomorrow’s workforce.
August 12, 2025
|

Leveraging Predictive Analytics to Navigate Uncertainty in Campus Workplaces
Predictive analytics is rewriting traditional campus planning rules, allowing institutions to design spaces that expand and contract with actual demand patterns.
August 12, 2025
|

Families Are Leaving Cities — Here’s How to Win Them Back
Children are critical to well-functioning cities. How can we ensure our cities work well for children and encourage parents to stay?
August 06, 2025
|

Designing for the Next Generation of Business Leaders
By investing in an experience-rich building, Purdue University’s Mitch Daniels School of Business aims to grow the next generation of business leaders and entrepreneurs.
August 01, 2025
|

How Strategic Shifts Can Reignite Employee Engagement
In today’s workplace, employee engagement isn’t just a buzzword — it’s a vital force behind organizational success.
July 30, 2025
|

Unlocking Value in Class A High-Rises: The Strategic Advantage of Spec Suites
In Class A commercial towers, spec suites are becoming a go-to strategy for converting vacancy into value.
July 30, 2025
|

Doing More With Less: Designing Small Spaces for Big Impact
Right-sized workplaces are redefining what it means to be effective — and proving that good design is measured not in square footage, but in experience.
July 28, 2025
|

3 Overlooked Human Factors That Make-or-Break Mergers and Acquisitions
Organizations that integrate people, culture, and physical space into their M&A strategy can unlock lasting value.
July 25, 2025
|

Reenvisioning Retail Centres: Lessons From China for the Middle East
We explore how key lessons from China’s retail evolution can reshape the future of retail centres in the Middle East.
July 23, 2025
|

Unlocking the Power of Forgotten Space to Combat Loneliness
By embracing the potential of empty space, reimagining in-between spaces, and extending the life of cities beyond traditional hours, we can unlock new value and bring people together.
July 21, 2025
|

The Power of Clean Air in Sports-Centered Design
In arenas, training centers, and stadiums, air quality is not just a comfort factor — it’s a competitive edge, affecting athletes’ ability to train, compete, and recover.
July 16, 2025
|

Al-Ahly Stadium Brings Fans Closer to the Action
Facing height and capacity restrictions, an innovative design solution turned these challenges into an opportunity to design a year-round, landmark sports venue.
July 10, 2025
|

Debunking 3 Myths About Generational Differences in the Workplace
As generational differences narrow, organizations should focus their workplace strategies across the entire talent spectrum.
July 09, 2025
|

The Evolving Role of Hotels in Retail-Driven Mixed-Use Environments
Hotels within mixed-use developments are becoming curated retail destinations and dynamic contributors to a vibrant urban experience.
July 07, 2025
|

The Rise of Outdoor Spaces at Airports
Major U.S. airports are actively incorporating outdoor terraces and patios as a passenger amenity — and transforming the traveler experience.
July 02, 2025
|

Airports Can’t Stop. Here’s How to Keep them Functional During Construction.
We share fresh optimism about how to improve the airport construction process. It starts with travelers’ experience as they pass through an airport with ongoing construction.
July 02, 2025
|

5 ‘Out of the Box’ Strategies for the Retail Real Estate Market
As big box retail closures mount, here’s a look at five unique uses to repurpose large, vacant spaces in a changing landscape.
July 02, 2025
|

Trends to Watch Shaping the Future of Airports and Aviation
Gensler’s aviation leader discusses what’s next for the future of air travel and how airports can cater to a new type of leisure traveler.
July 01, 2025
|

Urban Air Mobility Is Here. Here’s How Cities Can Adapt.
Advanced air mobility is ready for launch. The next crucial step: preparing buildings and infrastructure to get this sustainable mobility solution off the ground.
July 01, 2025
|

What Airports Can Learn From Stadiums and Ballparks
Here are six lessons from sports venue design to create a more seamless passenger experience.
July 01, 2025
|

Designing ‘the Quiet Airport’ at SFO
San Francisco International Airport (SFO) is helping to ease the passenger experience through hospitality-driven, inclusive design.
June 30, 2025
|

Building a New Temporary Home for Pali High
In the wake of L.A. wildfires, Gensler transformed a former Sears department store into a high school for 2,500 students in just four weeks.
June 25, 2025
|

How London’s Green Real Estate Can Lead the Global Climate Agenda
Despite global decarbonisation efforts, emissions continue to rise. But the UK is quietly and steadily reducing its carbon footprint.
June 20, 2025
|

Office-to-Hotel Conversions: Resilient Opportunities for Downtown Districts
Older and smaller Class B or C office buildings have been hit hard by high vacancy rates. Converting them to efficient, business travel hotels could offer an economical solution that supports the overall health of downtown business districts.
June 18, 2025
|

Belonging Begins at Home: Why Attainable Housing Is a Civic Imperative
We explore five strategies that demonstrate how design, policy, and planning can come together to build more inclusive, resilient communities.
June 17, 2025
|

The Top 10 Cities People Don’t Want to Leave
Gensler’s 2025 City Pulse survey reveals the top cities where people not only move to, but also stay long-term.
June 17, 2025
|

Historic Buildings: A New Solution for Modern Data Centers
Repurposing historic buildings into data centers is a compelling strategy for heritage preservation, sustainability, and digital transformation.
June 17, 2025
|
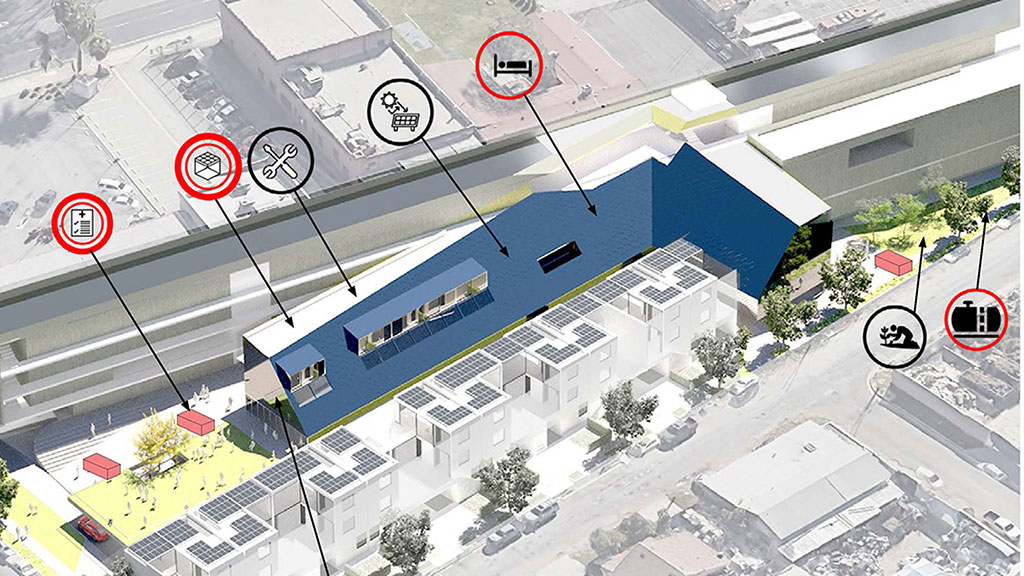
Reimagining Care in the Heart of Our Cities
An innovative intergenerational care concept seeks to transform how we support caregivers while revitalizing underutilized commercial spaces.
June 09, 2025
|

Libraries: The Last Urban Oasis
Libraries are no longer just a place for books; they play an integral role as the last bastion of democratic space in our cities.
June 06, 2025
|

How the Future of Work Is Influencing Workplace Design
While workplace design changes incrementally, the past few years radically transformed our expectations of an office and how we can design for what’s possible.
June 06, 2025
|
How Cities Can Establish Resilient Communities
To mitigate potential damage and risk, cities can form resilient communities to proactively prepare for, respond to, and recover from a disaster.
June 04, 2025
|

The Future of Work Is Human: Designing for Culture and Experience
The challenge in front of us is to design places that empower creativity, build belonging, and support people and teams to do their best work — whatever that looks like.
June 03, 2025
|

How a Challenging Site Fuelled a Bold New Workplace
A new building at The Goodsyard will transform an untapped site into a dynamic destination in London.
June 02, 2025
|

How the Nighttime Economy Is Rewriting Urban Design
Cities around the world are beginning to take the nighttime economy seriously — not as a separate or secondary system, but as a vital counterpart to daytime urban life.
May 28, 2025
|

The 20 Cities Attracting the Most Newcomers
New city residents often leave within five years. To remain successful, these magnetic cities must also engage and retain their new populations.
May 28, 2025
|

A New Vision for Urban Design in Tropical Climates
Through thoughtful, climate-responsive design, seemingly adverse conditions can become a distinct advantage for tropical cities.
May 28, 2025
|

A Surprising Reason to Feel Good About Returning to the Office
Why shared office space is a greener choice than working from home.
May 22, 2025
|

What Draws People to Cities — and What Makes Them Stay?
Gensler’s City Pulse 2025 research offers insights into the factors attracting people to cities and compelling them to stay.
May 21, 2025
|

The New Club Workplace: More Than an Amenity
The next generation of tenants wants an experience-driven, unconventional shared amenity space, prompting landlords to rethink their offerings.
May 15, 2025
|

The New Workplace Experiences That People Crave
Employees want to move past the corporate workplace experience to more creative, natural, and residential environments.
May 15, 2025
|

Designing an Eco-Retreat in Costa Rica’s Rainforest
Gensler Paris’ Managing Director explores how hospitality trends influence the design of this new Costa Rican resort — from the demand for cultural immersion to the rising appeal of slow travel.
May 15, 2025
|

Latin American Malls: The New Town Square
Malls across Central and South America are layered, experience-rich destinations that bring people together.
May 14, 2025
|

It’s Time for the Traditional Conference Room to Make Way for New Spaces
It’s time to forgo the traditional conference room and make space for more intentional, adaptable environments that are aligned with how people connect today.
May 12, 2025
|

Birmingham’s Renaissance: The City of 100 Quarters
How the city’s next evolution is embracing both innovation and heritage to shape a vibrant future.
May 08, 2025
|

How Summer FOMO Is Shaping the Canadian Workplace
Our latest research offers some insights into why a desire for flexibility, variety, and seasonal adaptability is influencing the workplace in Canada.
May 08, 2025
|

The Value of Time in Retail Environments
Time is a precious commodity, and brands that understand its value and choreograph both fast and slow retail experiences will thrive.
May 07, 2025
|

How AI Is Driving Innovation in the European Data Centre Market
The scale of data centre demand is driving innovations in energy generation, grid infrastructure, and cooling technologies.
May 07, 2025
|

Fusion Center Models: The Future of 24/7 Banking Support Hubs
In an increasingly digital world, banks are turning to Fusion Centers to protect and respond to cybersecurity threats, financial fraud, and other concerns.
May 06, 2025
|

How the AI Gold Rush Is Influencing Data Center Design Trends
Gensler’s Critical Facilities leaders discuss how the AI boom is influencing the shape, speed, and operations of data center design.
May 06, 2025
|

Lifestyle Living Is Redefining the Home in the Age of Belonging
We’ve identified five major trends shaping the future of living environments.
May 01, 2025
|

How Two Innovative Shelters Reimagine Refuge for the Homeless in Chicago
By prioritizing privacy and dignity, trauma-informed design can provide essential refuge and promote sustained healing.
April 30, 2025
|

How Law Firms in Mid-Tier Markets Are Leading Workplace Innovation
As law firms across the country reimagine the workplace, mid-tier markets are emerging as powerful leaders in this transformation.
April 29, 2025
|

Agency Is the New Workplace Amenity
By designing enough of the right spaces within the workplace, employers can create environments where employees have agency to choose the best space for their needs.
April 28, 2025
|

The Convergence of Tech and the Financial Workplace
The financial workplace is taking cues from the tech industry, shifting from one-size-fits-most to always-in-beta mode.
April 28, 2025
|

10 Opportunities for a More Resilient and Equitable Jersey City
Listening to the local community to improve climate justice, health, safety, and equity.
April 28, 2025
|

How Strategic Partnerships Are Shaping Academic Campus Development
Facing respective challenges, institutional-private sector collaborations can offer mutually beneficial opportunities for universities to expand their reach, optimize real estate, and enhance campus vitality, while providing developers with stable, high-value investment options.
April 25, 2025
|

Unlocking the Missing Middle: Why the U.S. Housing Model Needs a Redesign
How zoning, building codes, and financing reforms can unlock affordable, well-designed housing.
April 24, 2025
|

Why Now Is the Time for a Workplace Reset
To keep pace with changing workforce expectations, we need to think differently about the workplace.
April 24, 2025
|

Survivalist Architecture: The Age of Adapt & Reuse
Architecture must move beyond pure aesthetics to embrace solutions that prioritise environmental and social responsibility.
April 23, 2025
|
How to Design for Resilience
Resilient design is no longer a nice to have; it’s good business. Gensler’s Resilience Design report uncovers some key resilient design strategies.
April 22, 2025
|

Imagining a New Era for New Jersey’s Historic Art Factory
Originally built in the 1840s, the Art Factory is prime for a revitalization that preserves its character while serving the needs of a modern-day city.
April 16, 2025
|

The 18-Hour Campus: Strategies for Creating Vibrant, Round-the-Clock Hubs
Here are three strategies universities are adopting to create environments where students, faculty, and communities engage throughout the day and night.
April 14, 2025
|

How Design Drives Innovation in Education & Science
Gensler’s European Education & Sciences leaders explore how design can accelerate progress in these converging fields.
April 11, 2025
|

Urban Design’s Renaissance: How San Francisco Is Leading the Way
Cities everywhere are rethinking not just how they look and function, but how they can better serve the people who live in them. Few cities are as poised to lead this transformation as San Francisco.
April 09, 2025
|

5 Ways Suburban Office Campuses Are Transforming Into Thriving Communities
Tomorrow’s office campuses demand much more than a park and a café to attract and retain talent.
April 07, 2025
|

The Building as Brand: A Watershed Opportunity in Manhattan Office
As the city’s commercial real estate market undergoes unprecedented transformation, office space must be seen not as a commodity, but as a strategic investment with the potential to drive competitive advantage.
April 02, 2025
|

The Biggest Challenge to Office Conversions Isn’t Design — It’s the Status Quo
Office-to-residential conversions have the ability to unlock affordable housing and revitalize cities, but only if the market can move beyond the status quo.
April 01, 2025
|

Bandwidth Headquarters: A Workplace Designed Not Just for Work, But Life
An amenity-forward design approach cultivates a vibrant and dynamic workplace environment, empowering every employee to perform at their peak potential every day.
April 01, 2025
|

Live Event Amenities: The Next Frontier for Creative Workplaces
Companies are investing in live event-ready amenity spaces to attract talent, fuel creative work, and create buzz in the workplace.
March 31, 2025
|

What’s Next for the Workplaces of San Francisco?
As the city’s office market navigates recovery, landlords, building owners, and employers must consider the varying needs of future real estate vs. the status quo.
March 28, 2025
|

Why Now Is the Time to Double Down on the Promise of California Community Colleges
How these essential institutions could drive local, inclusive economic recovery.
March 26, 2025
|

How the Rise in Digital and Home Health Will Transform Healthcare
New technologies and digital tools leveraging AI are starting to redefine how we manage our personal healthcare needs — and it starts at home.
March 25, 2025
|
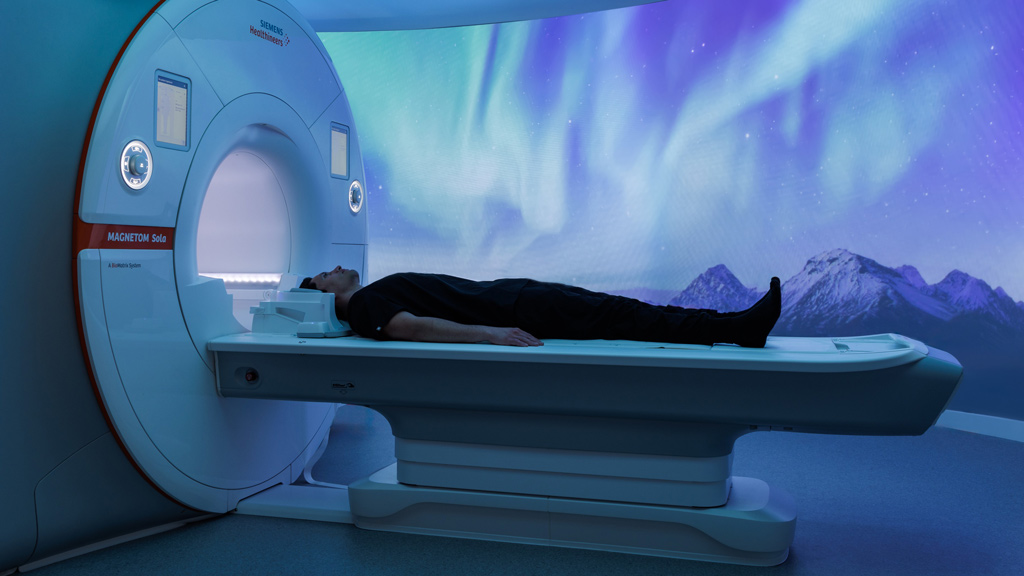
Realizing the Value of Artificial Intelligence When Planning Tomorrow’s Healthcare Facilities
The true value of AI lies not just in its ability to revolutionize devices and treatments but in its power to drive ROI through smarter, more adaptable healthcare environments.
March 24, 2025
|

Right-Sizing the Community Hospital: Optimizing for the Future
As U.S. health systems prepare for an uncertain future, our prototype hospital looks to expand care with fewer beds.
March 24, 2025
|

Trends to Watch Shaping the Future of Wellness
Gensler’s Wellness leaders discuss the opportunities shaping the future of wellness, from wellness real estate to inclusive design.
March 19, 2025
|

Reimagining Downtown: Transforming Underused Civic Buildings for a Vibrant Future
Former courthouses, grand banks, and other historic buildings at the center of our cities offer great potential to attract the public and activate our civic spaces.
March 17, 2025
|

Designing a New Future of Cities Through Wellness and Experience Design
How cities can take an active role in fostering healthier, more fulfilling urban lives for residents and visitors.
March 14, 2025
|

Creating a More Resilient Future With Green and Thriving Cities
As the demand for sustainable and liveable cities grows, urban planners and architects are adopting innovative strategies to harmonise built and natural environments.
March 13, 2025
|

Why Low-Carbon, Healthy Materials Are an Imperative for the Building Industry
Gensler’s updated Product Sustainability Standards™ aim to reduce the environmental impact of the building material supply chain, while driving industry change.
March 13, 2025
|

How Gensler’s Product Sustainability Standards™ Are Making an Impact in the Industry
We created the Gensler Product Sustainability Standards™ because we believe this is one of our most substantial opportunities for accelerating industrywide impact.
March 13, 2025
|

Introducing the Gensler Product Sustainability Standards™
We’ve set a new standard for all our projects to help increase demand for more regenerative materials in the building industry.
March 13, 2025
|

The Next Big Generation at Work May Not Be Who You Think
Historically, the fastest growing age group in the U.S. workforce has always been the upcoming generation. But not anymore.
March 12, 2025
|

Design Guidelines: The Most Powerful Tool in Your Real Estate Toolkit
Understanding a valuable tool that organizations can deploy to facilitate change in their real estate portfolio.
March 12, 2025
|

Healthier Spaces: Removing Harmful Chemicals From the Built Environment
Now is the time to take radical action and remove chemicals of concern from our buildings and spaces.
March 11, 2025
|

Three Principles for High-Impact Sustainable Design Guidelines
Translating sustainability commitments to design strategy.
March 10, 2025
|
Is Belonging the New Currency for Workplace Design?
By prioritizing belonging, we can create more impactful and transformative spaces that mitigate loneliness, foster connection, and drive value for people and organizations.
March 07, 2025
|

Designing for Flexibility in Senior Community Amenities
New insights in programming activities for tomorrow’s seniors will lead to the design of flexible, reconfigurable spaces and increased engagement.
March 06, 2025
|

How Branded Healthcare Environments Can Build Trust and Community
Brand identity plays a vital role in shaping patient experiences and reinforcing confidence in healthcare interiors.
March 03, 2025
|

Trends to Watch Shaping the Future of Senior Living Design
Gensler’s regional Northwest Senior Living leader discusses new housing models, amenities, and other opportunities shaping the future of senior living design
February 28, 2025
|

Why Resilience Planning Is Crucial to Safeguard Health Systems
Investing in proactive resilience planning, rather than reacting to weather and climate disasters as they unfold, will ensure uninterrupted, quality care.
February 27, 2025
|

Biodiversity as the New Frontier for Achieving Resilience in Real Estate
The biodiversity crisis is a fundamental challenge that impacts life, the global economy, and the real estate industry.
February 25, 2025
|

The Future of Mixed-Use Communities in Phoenix
Phoenix is well positioned for continued expansion, capitalizing on new technologies, sustainable practices, and architectural innovation.
February 20, 2025
|

Repopulating the Workplace: Why Collaboration Space Is in Danger
Despite their value, collaboration spaces are often the first to go when companies are looking for ways to repopulate the workplace.
February 18, 2025
|

The New Experiential Hybrid
The New Hybrid experience brings together the robust attributes of commerce, culture, and leisure, and recalibrates the urban experience.
February 11, 2025
|

The Uncertainty of Electric Power: A View from Houston
Through innovative design, regulatory support, and community participation, we can enhance our resilience to extreme weather events and ensure a more stable energy supply.
February 07, 2025
|

The Future of Lab Automation: Opportunities, Challenges, and Sustainable Design Solutions
Automation in labs isn’t just about advanced tools; it’s about creating an ecosystem that considers workflow efficiency, spatial design, and environmental sustainability.
February 07, 2025
|

How Repositioning Houston’s Astrodome Can Serve as a Model for Aging Sports and Entertainment Venues
A proposal to redevelop and repurpose the iconic stadium into a multi-use venue would preserve the building’s historic integrity while giving it new life.
January 31, 2025
|

What Do Consumers Want? Gensler’s U.S. Consumer Experience Report Uncovers Key Insights
Gensler’s latest consumer research delves into how design can impact human experiences for the better.
January 31, 2025
|

Communicating Sustainability: Quantifying, Qualifying, and Celebrating Climate Impact Achievements
Wherever a company or brand may be on its sustainability journey, telling the story of impact in a way that is both authentic and transparent is increasingly crucial.
January 30, 2025
|

A Radical Solution to the U.K. Housing Crisis: Building a New London in the Thames Estuary
How should the U.K.’s government be addressing the housing crisis? Here are four steps to a radical solution.
January 29, 2025
|

Trends to Watch: What Other Cities Can Learn From New York City’s Conversion Boom
As U.S. cities experience high commercial real estate vacancy rates and housing shortages, developers have an opportunity to invest in and convert stranded assets.
January 29, 2025
|

What Retail Can Learn From Chinatown: 3 Ways to Create Thriving Third Places
Looking towards San Francisco’s Chinatown as a case study, here are three key strategies to create a thriving third place.
January 29, 2025
|

What Are Corporate Real Estate Executives Planning for 2025?
A look at what office space portfolio modifications and space allocation strategies CRE leaders are anticipating and planning for the year ahead.
January 27, 2025
|

The Future Is Mixed Use: How Principles of Mixed Use Design Will Restore Our Communities
Here are four principles for creating mixed-use environments that will future-proof real estate.
January 27, 2025
|

The New Era of Retail Banking Is Here
To stay relevant, banks must transform branches into spaces that go beyond transactions, creating experiences that resonate with a new generation of consumers.
January 21, 2025
|

5 Design Considerations for Authentic Specialty Market Experiences
Though the retail and dining sector has struggled with pandemic recovery and rising costs, the specialty markets subcategory is thriving.
January 21, 2025
|

The Future of Healthcare Is Anchored in Its Communities
Community health hubs will play a vital role within an integrated ecosystem of health and care.
January 17, 2025
|

3 Ways Gensler Is Designing for a Zero-Carbon Future
The most successful buildings of the future will contribute to the well-being of the environment while bringing their carbon emissions to zero.
January 16, 2025
|

Why Quality in Commercial Office Space Hinges on Workplace Experience
Demand is surging for premium office environments that deliver an effective workplace and a great work experience.
January 14, 2025
|

Designing a Community-Based Workplace for Valley Bank
Gensler partnered with SJP Properties and Valley Bank to envision both the base building and a community-driven workplace interior for Valley’s employees.
January 13, 2025
|

Avoiding Fear-Based Decision-Making to Foster Positive In-Store Retail Experiences
How deliberate design decisions can boost brand recognition and connect with customers.
January 10, 2025
|

Removing Behavioral Health Stigmas Through Elevated, Strategic Design
We designed a revolutionary new kind of emergency facility to break down social and systemic barriers surrounding behavioral health care.
January 09, 2025
|

The Future of Energy: How Small Modular Reactors Are Changing the Game
As the global demand for energy soars, small modular reactors are emerging as a key player in the race to meet this need with clean, efficient power.
January 08, 2025
|

How Gaming Can Transform Activation and Transition Planning for New Healthcare Campuses
A gamified approach to training can help educate and engage staff when transitioning to new healthcare facilities.
January 08, 2025
|

How AI and Emerging Technologies Will Transform the Future of Labs
From AI and machine learning to quantum computing, we explore how technological advancements are redefining how scientists work.
January 07, 2025
|
Bringing Spaces to Life: The Integral Role of Service Design in the Design Process
Service design acts as a bridge that connects the physical design of a space with the user-centric experiences within it.
January 07, 2025
|

When It Comes to Workplace Design, Beauty Drives Performance
Beauty plays a crucial role in driving workplace performance, going beyond mere aesthetics to shape overall functionality and impact the employee experience.
January 06, 2025
|
A Field Guide to Authentic Amenities
To create authentic amenities that workers truly want, designers and companies should think outside the box.
December 19, 2024
|

The Campus as a Catalyst: Combining Student Needs With Institutional Goals
Here are some key strategies for differentiating a university campus, improving retention, and reimagining underutilized spaces to optimize real estate.
December 17, 2024
|

A New Approach to London’s Dated Offices
To revitalise London’s dated office building stock, we must make these environments relevant and capable of attracting the best tenants and talent.
December 16, 2024
|

Workplace as a Service: A Thought Experiment in Office Evolution
The concept of Workplace as a Service challenges traditional notions about work environments. Will this new design perspective help the office remain relevant?
December 12, 2024
|

Trends to Watch: The Future of Entertainment in the Built Environment
Gensler’s Entertainment leaders discuss the opportunities shaping the future of entertainment, from immersive experiences to entertainment districts.
December 11, 2024
|

Trends to Watch: The Future of Cities Relies on Multiuse Districts
Gensler’s Mixed Use & Retail Centers leaders discuss the opportunities shaping the future of cities and multiuse districts.
December 10, 2024
|

Trends to Watch Shaping the Future of Mobility and Transportation
Gensler’s mobility and transportation leaders discuss the biggest trends shaping the industry, from micromobility to electrification.
December 10, 2024
|

Trends to Watch: Building City Identities to Become Destination Brands
How can brand positioning and a compelling narrative help cities create global destinations and build strong brand advocates?
December 06, 2024
|

Trends Shaping the Industrial Market in Latin America
We explore some of the key trends, innovation, and strategic design shaping the industrial sector in the region.
December 05, 2024
|

Design for Laboratory Resilience: A Compliance Approach to Climate Risk Assessment
Innovative sustainable design of laboratory buildings must factor in risk of regional natural disasters and affected communities.
November 22, 2024
|

The Secret to Paris 2024’s Olympic Success? Reuse, Temporality, and Legacy
How an innovative, sustainable, and cleverly timed approach helped Paris avert the pitfalls many cities face when hosting the Olympic Games.
November 22, 2024
|

How Communities Can Benefit From Mixed-Use Data Center Integration
As suburban communities restrict new data centers, innovative master planning development is challenged with integrating critical facilities into mixed-use settings.
November 13, 2024
|

Designing for the Future of Theater and Immersive Entertainment
Our Media and Entertainment leaders discuss what’s next for immersive theater and performing arts venues.
November 12, 2024
|

Climate Resilience in the Latin American Caribbean: Challenges and Opportunities
To mitigate the effects of climate change in the region, we must adapt cities, strengthen infrastructure, and protect vulnerable communities.
November 12, 2024
|

Office-to-Residential Conversions: What Boston Can Learn From New York’s Momentum
New York City’s conversion success story offers valuable lessons for Boston as it seeks to address its own housing shortage amid a surplus of office space.
November 11, 2024
|

Realizing Virsona’s Vision for Interactive, Community-Driven Gaming Spaces
Gensler and social gaming startup Virsona discuss the opportunity to create in-person communal spaces for one of the country’s most popular pastimes: video games.
November 11, 2024
|

How Immersive Food and Beverage Experiences Are Redefining Hospitality
Food and beverage spaces have unique potential as experiential destinations that authentically convene community in a way that is familiar, universal, and transformative.
November 06, 2024
|

Trends Shaping the Future of Retail in Latin America
Embracing cultural identity, technology, and sustainability is key to engaging consumers in the region.
November 04, 2024
|

Reimagining Digital as an Enhanced Building Material
As technology becomes more invisible, we are merging physical and digital experiences to redefine how digital is considered in the built environment.
November 04, 2024
|

The Powerful Influence of Experience Design in Transforming Retail
The intersection of retail and experience design yields curated atmospheres that foster community connection and strengthen brand loyalty.
November 01, 2024
|

Redefining the Workplace for a New Era of Productivity and Engagement
This new era of work is not about obligation but about crafting a compelling experience that draws people in and encourages them to grow personally and professionally.
October 30, 2024
|

10 Workplace Trends for 2025: What’s In and What’s Out?
The workplace is evolving beyond a collection of experiences and becoming a space designed to foster intentional transformations.
October 30, 2024
|

What Two Mixed-Use Districts Reveal About Successful Retail and Placemaking
Lessons from two mixed-use destinations in Texas reinforce the value of adaptability and careful placemaking for large, retail-centered developments.
October 29, 2024
|

Face-to-Face Work and Aging Building Stock – How Can We Make Sense of French Workers’ Contradictory Attitude Towards Their Office?
There is an inextricable paradox in the attitude of French workers towards their workspaces.
October 17, 2024
|

4 Considerations for Implementing a Better Self-Checkout Experience
When done right, self-checkout can improve efficiency without sacrificing experience.
October 16, 2024
|

Designing Workplaces to Strengthen Connection and Combat Loneliness
The workplace plays a key role in fighting against the growing loneliness epidemic.
October 15, 2024
|

How Your Workplace Can Supercharge Performance
What workplaces can learn from the gym and the football pitch about creating environments that inspire workers to stretch, develop, and achieve.
October 10, 2024
|

The Evolution of Sports Venue Brand Integration: From Simple to Sophisticated
The new landscape of brand in sports is more sophisticated than ever.
October 09, 2024
|

Gensler Voices: Ariadna Hernandez on Design’s Greatest Strength
Ariadna Hernandez, a designer for Gensler Washington, D.C., shares how design can improve lives from multiple angles.
October 09, 2024

Architects Must Design for a New Age
For the first time in the history of our profession, architects are now outliving their buildings. How can we design with impact and keep up with the rapid speed of change?
October 08, 2024
|

Smart Design for Smart Manufacturing: Five Ways Manufacturing Has Evolved
In a market poised for significant growth, these markers of change present opportunities in both the near and long-term.
October 08, 2024
|

Emerging Trends in Climate Action From Climate Week NYC
Signals that the climate dialogue is evolving to meet the urgent need for impact at scale.
October 03, 2024
|

Using Narrative Design and Local Context to Create Authentic and Memorable Hospitality Experiences
Gensler's global leaders for Hospitality and Experience Design discuss the intersection of these two industries and their process for creating memorable destinations.
October 02, 2024
|

A Story of Transformation: Hyatt’s Unique Blend of Community and Hospitality
Strategies for repositioning an aging hotel ground floor into a community destination.
October 01, 2024
|

What Spa and Wellness Spaces Can Teach Us About Transforming Behavior
Luxury hospitality and spa experiences are leading the charge in changing how we experience and interact with technology.
October 01, 2024
|

The Perpetual Asset: Design for an Evolving Market
What if we could diversify a real estate portfolio with just one building?
September 25, 2024
|

Expanding New Frontiers: Redefining Hospitality in Latin America
From personalizing experiences to deepening cultural immersion, here’s how hospitality is evolving in LATAM.
September 25, 2024
|

Gensler Voices: Cristina Ziegler McCoig on Communities and Design
Cristina Ziegler McCoig, a designer for Gensler San Antonio, shares how a focus on local aligns with universal design principles.
September 25, 2024

Gensler’s D.C. Office Expansion, Renovation, and a Groundbreaking New Way to Break Down Broadloom Carpet
An office expansion pushes ideals around material reuse in a circular economy, sustainability, and workplace design.
September 23, 2024
|

Quantity and Quality: Leveraging Office-to-Senior Living Conversions to Increase Capacity and Lifelong Well-being
Office-to-residential conversions have helped reduce vacancy rates and unlock housing. It’s time to repurpose the solution to meet the growing demand for senior living.
September 23, 2024
|

Four Big Takeaways From Gensler’s New Global Climate Action Survey
What is the state of climate change perceptions in 2024?
September 18, 2024
|

Regional Revitalization: Designing for Impact in the Middle East
Tim Martin, former Gensler Middle East Managing Director and Steven Velegrinis, Gensler Middle East Design Director, discuss designing for the region’s revitalization opportunity.
September 17, 2024
|

The Shift to Extremes: Rethinking Office Design
Modern offices are increasingly designed with extremes in mind, featuring specialized spaces for both hyper-focus and hyper-collaboration.
September 13, 2024
|

The Future of D.C. as the Capital of Creativity
A conversation on the shifts and opportunities that could transform our nation’s capital and redefine its role on the global stage.
September 12, 2024
|

Five Benefits of Leaning into Brand Identity and Culture for Office Design
Learn how Synopsys’ new workplace drives productivity and connectivity.
September 12, 2024
|

The “Mental Load” and Its Effect on Athlete Performance
We can help reduce athletes’ mental load by including specific amenities in training facilities and giving them the space and time to focus on being at the top of their game.
September 12, 2024
|

Gensler Voices: Francesca Alchanati on The Profound Impact of Design
Francesca Alchanati , a designer for Gensler Washington, D.C., shares how design can help spaces be inclusive for all.
September 12, 2024

Designing Safe, Walkable Cities for Future Generations of Children
Thoughtful urban design can transform cities into vibrant, inclusive spaces where children can thrive, connect, and grow.
September 11, 2024
|

How Large, Adaptable Multi-Purpose and Event Spaces Are Transforming the Financial Services Workplace
Major financial institutions are incorporating large, multi-purpose event spaces into their new office designs — even in cities where square footage comes at a premium.
September 05, 2024
|

How to Create a Multigenerational Workplace
Here are six strategies organizations can use to cultivate environments where individuals of all ages feel valued, engaged, and empowered.
September 05, 2024
|

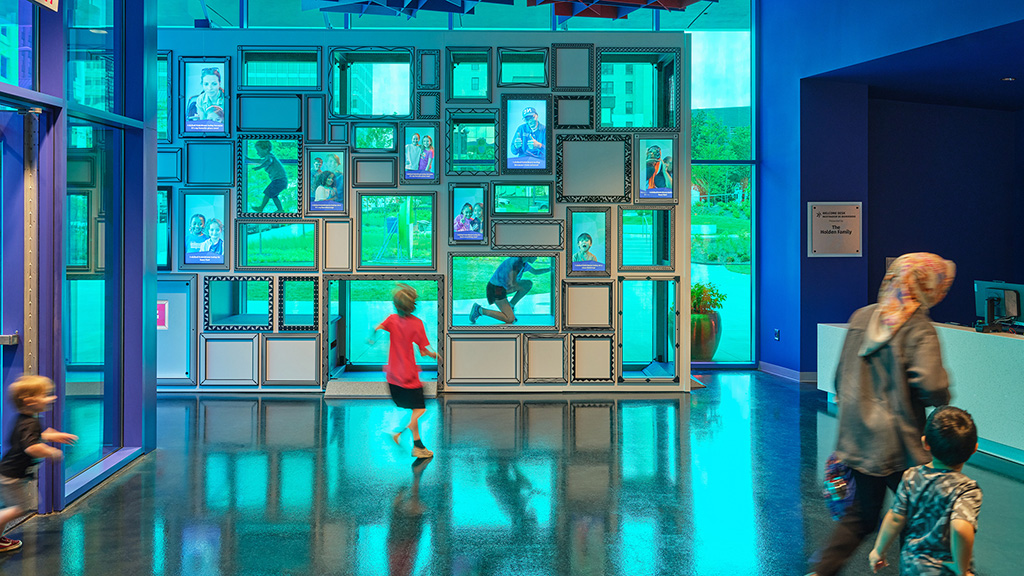
Bringing Community to the Community Center
In Houston, Gensler helped reimagine the Evelyn Rubenstein Jewish Community Center as a place that celebrates the Jewish community in every moment.
September 04, 2024
|

Imagining a Smart Recycling Reward System That Transforms the Way We Look at Trash
By transforming recycling into a rewarding, interactive process, we can inspire collective action to revolutionise waste management.
September 04, 2024
|

Beyond the Screen: Exploring the World of Museums and Experiential Technology
Digital experiences in museums, exhibits, and other interpretive spaces go beyond the screen for dynamic and memorable storytelling.
September 03, 2024
|
Creating a Range of Entry Points to Engage New Museums Audiences
Our Culture & Museums and Entertainment and Experience Design leaders to discuss what’s next for museums and cultural spaces.
September 03, 2024
|

The Evolution of the Museum
Unlike the institutions of the past, modern museums can flourish and differentiate themselves by being more forward-looking, community-driven, dynamic, and engaging.
September 03, 2024
|

Gensler Voices: Meredith Flanagan on Life at Gensler Beyond Design
Meredith Flanagan, a workplace experience manager for Gensler Washington, D.C., shares her perspective creating experiences for her Gensler office.
August 29, 2024

Conversions for Healthcare:
10 Takeaways for the Future
As healthcare systems shift to a new model of distributed care, adaptive reuse of older buildings will be an important strategy to sustainably achieve their goals.
August 27, 2024
|

Creating Inclusive Spaces by Designing for Neurodiversity
Designing for neurodiversity is an essential evolution in our drive to craft inclusive environments that support productivity, well-being, and employee satisfaction.
August 22, 2024
|

The Impact of Inclusive Design on Children’s Health and Happiness
By using inclusive design strategies in city and urban planning, we can build spaces that allow children to flourish, learn, play, and grow.
August 21, 2024
|

Uncovering Growth: Wellness Real Estate Across the Market
An increased emphasis on physical, emotional, and social health has had a significant impact on the goods, services, and spaces that support peoples’ overall well-being.
August 21, 2024
|

Insights Into the Pandemic’s Impact on Student Well-Being
Our research explores how the shift out of the pandemic is impacting student relationships, motivation, and emotional well-being.
August 21, 2024
|

6 Solutions for Designing a More Inclusive Workplace
In today’s changing work landscape, it’s critical to design environments where everyone feels safe, supported, and welcome.
August 16, 2024
|

Inclusive Design for the 21st Century Library
Exploring strategies to create universally welcoming and functional libraries that cater to their communities.
August 16, 2024
|

Learning on the High Street: A Vision for the Future
Addressing digital inequality is vital to improving educational outcomes and influencing future innovation, economic prospects, and societal well-being.
August 14, 2024
|

Are Educators and Campus Staff Ready for an Unassigned Workplace?
In the age of hybrid work, campuses have an opportunity to explore new approaches to workspace, specifically shared and unassigned space for staff and educators.
August 13, 2024
|
A New Tool Helps Organizations Maximize Their Community Impact
Gensler’s Urgency Index helps institutions make informed decisions that amplify their impact by locating in the communities that need them most.
August 13, 2024
|

How Urban Design and Educational Spaces Can Combat Child Loneliness
Through thoughtful urban design, we can create inclusive, supportive environments where children can safely explore and learn outside traditional classroom settings.
August 12, 2024
|

Reflecting on the Paris 2024 Olympics: A Catalyst for Urban Transformation and Sustainability
A look at how the key trends emerging from the 2024 Summer Olympics are creating a more inclusive and sustainable future for sports and urban development.
August 09, 2024
|

A New Story of Design Starts in Monterrey, Mexico
With its vibrant academic scene and growing industrial and logistic businesses, Monterrey is one of the bright spots in a booming Mexican economy.
August 07, 2024
|

A Future-Proofed Garage in the Heart of Silicon Valley
Near Google’s headquarters in Mountain View, Alta Garage was designed with a second life in mind — one that is not limited to parking.
August 06, 2024
|

How Modern Training Centers Can Shape Tomorrow’s Champions
Helping athletes achieve their best, training centers and human performance labs (HPLs) are playing more important roles than ever to support competitors.
August 05, 2024
|

The Power of Trust in Experiential Design
Humans have a deep biological need for safety, and when we design for this need, it lets us also design for an experience of emotion that leads to meaningful human connection.
July 31, 2024
|

Worldbuilding: Creating Transformative Experiences With Narrative Design
When narrative is leveraged as a tool for design, it helps to drive emotional connection and the sense of a shared experience.
July 31, 2024
|

How the Olympics and Paralympics Can Shape Cities in New Ways
A look at the legacy, equity, and sustainability shaping the Games, and how this event can unlock a city’s future potential while showcasing it in novels ways.
July 31, 2024
|

The 5 Attributes That Define an Immersive Experience
When successful, immersive experiences give people a chance to connect deeply with the present moment and with others around them.
July 30, 2024
|

Conversations on the Intersection of Design and Disability Inclusion
Members of ADAPT, Gensler’s affinity group for disabled and/or neurodivergent staff share how design, and working in the industry, can be more inclusive for all.
July 30, 2024
|

Data Keeps Us Going:
How Data Centers Power Society
In today’s digital age, data, and data centers, have become as essential a utility as electricity or water.
July 29, 2024
|

The “Five I’s” of Design
By embracing imagination, initiative, inclusion, intention, and impact, we can elevate the human experience through design.
July 26, 2024
|

How Technology Is Redefining the Fan Experience at Sports and Music Venues
In this Q&A, our Digital Experience Design and Sports leaders discuss how technology is currently being used to streamline venue operations and enhance the fan experience.
July 24, 2024
|

Gensler Voices: Justin Rankin on The Duty of Design
Justin Rankin, a practice area leader for Gensler Austin, shares more about habits and design impact.
July 24, 2024

Elevating the “Standing Room Only” Fan Experience in Sports Venues
In recent years, sports design focused on the premium fan experience. But how can we cater to the standing-room only crowd and make them feel part of the venue experience?
July 23, 2024
|

Small Upgrades, Big Impact: How Sports Facilities Can Enhance the Fan Experience and Deliver ROI
Smaller projects within a sports facility create opportunities to keep a stadium fresh and transform fan experiences in targeted ways.
July 23, 2024
|

Reimagining North Michigan Avenue: A New Era for Chicago’s High Street
Gensler’s study envisions a series of interventions to create an engaging experience on one of the world’s most iconic high streets.
July 18, 2024
|

Tech Is Broadening Its Impact by Embracing Communities
To appeal to top talent, tech companies have pushed their focus beyond their workplaces to embrace their surrounding neighborhoods.
July 18, 2024
|

Designing with Intention: Creating Emotional Connections Through Immersive Experiences
In this Q&A, Gensler’s global leaders of Digital Experience Design and Entertainment unpack the concept of experiential architecture and what makes an immersive experience.
July 17, 2024
|

Gensler London’s Commitment to a Sustainable Workplace
New to the U.K. market, the NABERS Tenancy Certification aims to help owners and tenants measure their buildings’ environmental performance and identify areas for improvement.
July 17, 2024
|

The Future of Workplace Experience Is Here: How AI Is Transforming Spaces
The advanced integration of AI into physical environments has the potential to reimagine spaces as more efficient, connective, and inspiring.
July 16, 2024
|

How the Tech-Enabled Workplace Can Create Better Hybrid Experiences
How can we design workspaces that benefit everyone, regardless of whether they have a seat at the conference room table?
July 16, 2024
|

Be Bold Not Beige: The Power of Colour to Shape Everyday Experiences
From boosting productivity in the workplace to soothing the soul at home, colour can transform the places where we live, work, and play.
July 12, 2024
|

Office-to-Residential Conversion: A New Value Proposition for the German Market
This adaptive reuse strategy represents a value proposition that could help the country meet housing demand and achieve decarbonisation goals.
July 02, 2024
|

How Design Can Integrate Social Value Into Residential Developments
Design plays an integral role in fostering social value within residential areas.
July 02, 2024
|

Maximizing Building Portfolio Value: The Crucial Role of Lease Support Services and Up-to-Date BOMA Records
Lease support services are no longer a nice-to-have but a necessity for building owners and managers to stay ahead in the competitive real estate market.
June 28, 2024
|

Trends to Look for at the 2024 Summer Olympics and Paralympics
How Paris 2024 is achieving more with less, and the trends shaping the Games wide open.
June 27, 2024
|

Maximising Urban Space: 3 Strategies for Solving the U.K.’s Housing Crisis
Addressing the U.K. housing shortage will require a multifaceted, strategic approach, recognising the urgent need for land to accommodate new homes and infrastructure.
June 26, 2024
|

Gensler Voices: Abbey Rampy on Following Her Gut
Abbey Rampy, a designer for Gensler Charlotte, shares the best career decision she’s made.
June 26, 2024

Design as a Superpower in the Senior Living Industry
Excellent design of senior living facilities prioritizes well-being in ways that should be automatic for all types of design.
June 26, 2024
|

Laying the Groundwork for Climate Preparedness
Gensler’s Resilience Preparedness Framework develops concrete actions that designers can take to address climate shifts.
June 24, 2024
|

Designing the Future Workplace for a Growing Professional Services Firm
How a collaborative design partnership evolved this national accounting, tax, consulting, and business advisory firm’s workplace experience.
June 24, 2024
|

Prototyping the Hospital of the Future
By prioritizing critical care, streamlining support services, and designing for long-term adaptability, hospitals can create a more sustainable future for healthcare.
June 21, 2024
|

Navigating Federal Resources for Office-to-Residential Conversion
As building owners in the U.S. face the prospect of defaulting on office buildings, many are turning toward the federal government for a financial lifeline.
June 18, 2024
|

San Francisco Is on the Brink of a Revival, Fueled by AI, Innovators, and Investors
Contrary to reports of the city’s demise, more people are feeling satisfied with their living experience.
June 18, 2024
|

Luxury + Convenience: Why Branded Residences Are in Demand Across the Globe
In the residential sector, we’re seeing an increased demand for high-end, branded residences that offer hotel-style services and amenities.
June 17, 2024
|

Pearl House: Explore the Transformation of New York’s Largest Office-to-Residential Conversion to Date
Gensler and Vanbarton Group detail how they partnered to convert a 1970s office tower into a thriving residential community in New York’s Financial District.
June 12, 2024
|

Are ‘New Towns’ the Solution to the U.K. Housing Crisis?
The U.K. is struggling to provide enough housing for its growing population. Now is the time for a more radical approach to the provision of housing.
June 10, 2024
|

The Pandemic Hit New York Hard — But Its Recovery Has Been Swift
Despite facing significant challenges, New York City’s economic recovery showcases its resilience and durability in the face of disruption.
June 05, 2024
|
The Importance of ‘Carbon Storytelling’ in Future Sustainable Architecture
‘Carbon storytelling’ will be essential for sustainable buildings of the future — here’s why.
June 05, 2024
|
Gensler Voices: Jonathan Plass on How Listening Can Bring Inspiration
Jonathan Plass, a design analyst for Gensler Washington, D.C., shares his career journey in design from early influences to his favorite projects.
June 05, 2024

What’s the Recipe for Retail Success? Food
With a heightened consumer appetite for engaging social spaces, food and beverage are key ingredients for physical retail viability.
June 04, 2024
|

An Innovative Solution to Confront Mexico City’s “Day Zero”
A visionary project seeks to redefine Mexico City’s relationship with water, offering a beacon of hope in the face of scarcity.
June 04, 2024
|

From Mill Towns to Cities: How the Mass Timber Revolution Is Impacting People and the Planet
What if there was something the design industry could do to revitalize rural communities with access to abundant, renewable forest resources?
May 31, 2024
|

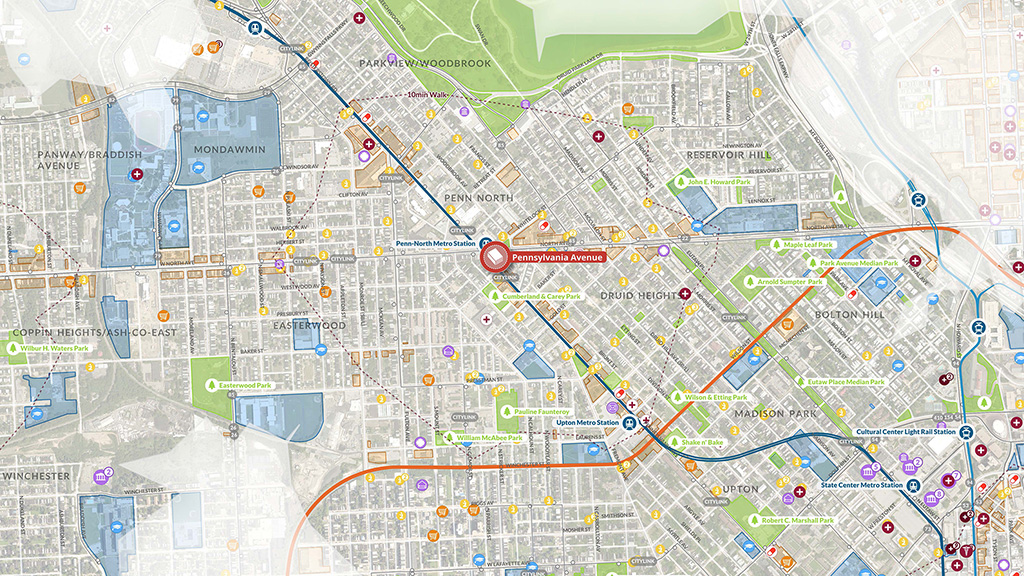
Introducing the Gensler Transit-Oriented Development Opportunity Index
The Gensler Transit-Oriented Development (TOD) Opportunity IndexTM is a tool for unlocking the unrealized value of existing transit stations and facilities.
May 31, 2024
|

Why Singapore’s Flexi-Time Regulations Are a Step Towards Building a More Sustainable Work Culture
New government regulations are shifting to meet the evolving needs of the country’s workforce.
May 29, 2024
|

Trends to Watch: How Media Workplace Priorities Have Evolved in 2024
Gensler’s latest research and project work has uncovered new ways the design of the media workplace can deliver what employees want and need in an office experience.
May 28, 2024
|

Why Hospitality Must Adopt the “Leave No Trace” Mindset
By embracing “Leave No Trace” ideas, we can raise the bar on placemaking that brings people together, elevates natural and urban spaces, and preserves the Earth.
May 23, 2024
|

How Public Libraries Are Building Community
The public library’s mission has changed from a simple repository to a community center, where learning experiences, cultural resources, and community interaction take place.
May 22, 2024
|

Mexico City Is Reckoning With Explosive Economic Growth Alongside a Mounting Water Crisis
Despite an influx of capital and accelerated economic growth, Mexico City is grappling with a water shortage and affordability challenges.
May 22, 2024
|

Equitable Public Engagement for a Changing World
Equitable outcomes begin with an equitable process, and public engagement is key.
May 21, 2024
|

Singapore’s Recovery Is Challenged by High Housing Costs
Learn what Gensler’s City Pulse research reveals about how Singapore has rebounded since the pandemic.
May 16, 2024
|

Want a High-Performing Workplace? Here’s What Matters Most.
Our research identifies what makes a high-performing workplace and what design factors matter most.
May 15, 2024
|

How Workplaces in Tokyo Are Embracing Flexible Work
Tokyo is embracing flexible work to support a diverse workforce and companies are taking careful steps to design workplaces that meet modern expectations.
May 15, 2024
|

Inclusive Product Design
Should Never Exclude Style
Products that are ADA compliant are typically well-engineered, but often bulky, institutional in appearance, and emotionally dispiriting — and millwork pulls are no exception.
May 15, 2024
|

The Key to a Better Workplace? Understanding How and Where People Work Today
Our global workplace research uncovers insights into how new work patterns can help design better workplaces for the future.
May 13, 2024
|

Writing the Next Chapter of Sports and Entertainment in Kansas City
Co-CEO Jordan Goldstein and Studio Director Greg Brown detail the evolution of sports and entertainment design and why expanding into this market offers unmatched opportunity.
May 13, 2024
|

What Can San Francisco Learn From Successful Building Conversion Programs in Other Cities?
By taking cues from other cities, San Francisco has an opportunity to make it easier to repurpose buildings, address the housing crisis, and revitalize downtown.
May 08, 2024
|

What’s on the Horizon for Low-Carbon Design in the U.K.
In the last five years, the way we think about carbon in our buildings has transformed — but the biggest impacts are yet to come.
May 07, 2024
|

Post-Pandemic, London Is Drawing Back People, Jobs, and Businesses
Gensler’s City Pulse Retrospective suggests that “boomerang Londoners” are returning to London for social, cultural, and career opportunities.
May 03, 2024
|

What Gensler’s Education Engagement Index Reveals About the Future of Hybrid Learning
An exploration into the future of the hybrid learning experience.
May 02, 2024
|

Gensler’s City Pulse Retrospective Tracks the Complex Shifts in Urban Life
Our latest cities research reveals that despite pain points, the desirability of cities persists.
April 30, 2024
|

Innovations in Mobility Design Are Paving the Way for More Resilient Cities
The way people travel in, around, and between cities affects everything from urban planning to sustainability, and design plays a key role in supporting new behaviors.
April 30, 2024
|

The Most Impactful Urban Infrastructure? City Streets
Gensler’s plan for Hollywood Boulevard demonstrates how rethinking city streets can revitalize cities, create healthy communities, and support sustainable mobility.
April 29, 2024
|

Beyond the Property Line: How to Design a Sustainable Material Supply Chain
We have a tremendous opportunity to think beyond the property line and holistically address impacts from the interconnected, global system of building materials.
April 25, 2024
|

Invisible Cities: Mitigating the Bird Strike Problem
With proper research and active measures, we can help solve the bird strike problem and benefit ecosystems across the globe.
April 25, 2024
|

Using Design to Bring Hope
As design professionals, how do we incorporate positive and equitable impacts into our design? How can we use the power of design to change lives and heal communities?
April 24, 2024
|

Gensler Voices: Shirin Masoudi on Her Design Inspiration
Shirin Masoudi, a designer for Gensler Seattle, shares her unique perspective on design.
April 17, 2024

4 Powerful Approaches for Putting Climate Goals to Action
We’ve identified four approaches that put organizations on a credible path to achieving climate goals.
April 16, 2024
|

Driving Sustainability Through Digital Experience Design
By lowering energy consumption, reducing e-waste, and elevating eco-friendly materials, digital experiences can become an asset in sustainability messaging.
April 16, 2024
|

Using an “All-Spokes” Approach to Optimize Lab Space
It's not just a question of space, but rather the nexus of space, people, process, operations, equipment, and technology.
April 16, 2024
|

Decarbonizing the Built Environment for a More Sustainable Future
By acting quickly and working with industry partners to develop and promote lower embodied energy materials, we can catalyze a low-carbon marketplace.
April 15, 2024
|

5 Things Developers Should Know About Mass Timber
With its inherent structural integrity and positive impact on carbon emissions, mass timber can make a big impact in tackling climate action in the built environment.
April 09, 2024
|

Global + Local Design Is a Powerful Tool for Navigating Change
At a time when deglobalization is on the rise, the role of design as an integrator has never been more critical.
April 05, 2024
|

BOMA 2024: 5 Key Changes Reshaping Office Building Measurements
Here are five improvements you need to know about the new BOMA 2024 office standard.
April 04, 2024
|

A Football Academy Designed to Empower Youth in Ghana
Right to Dream’s Ghana campus is a best-in-class facility that sets a benchmark for football academies everywhere.
April 03, 2024
|

Gensler’s Mexico City Office: A Model for the Future Workplace
A model of workplace transformation, Gensler’s new Mexico City office blends authentic Mexican culture with forward-thinking design principles.
April 02, 2024
|

Decarbonization Needs to Hit Closer to Home
If cities want to get serious about reducing their carbon impact, exploring ways to reduce the emissions of our homes is a key opportunity.
April 02, 2024
|

A Well-Designed Workplace Is a Competitive Advantage
A healthy, sustainable workplace acts as a magnet for talent — and sets a property apart in today’s competitive market.
April 02, 2024
|

Revolutionizing Child Care: The Key to Enhancing Your Return-to-Office Strategy
By offering on-site or nearby child care options, businesses can position themselves as employers of choice.
April 01, 2024
|

Trends to Watch Reshaping the Future of Cities and Urban Living
Gensler’s Cities & Urban Design leaders discuss what’s next for the future of cities.
March 29, 2024
|

Trends Shaping Sports Venue Design in the European Market
Gensler Sports leaders discuss what’s next for stadium and training facilities in Europe, and key opportunities for growth in the European market.
March 28, 2024
|

Rethink, Redirect, and Rewild: Nature-Based Design Solutions for Carbon Sequestration
By utilizing nature-based design solutions to rethink carbon sequestration in our work, we have an opportunity to make a positive impact on our net zero goals.
March 27, 2024
|

A Fresh Take on the Corporate Workplace, With Inspiration From 19th Century London
With its historic character, Francis House provided the perfect platform to create a dynamic, engaging, and holistic employee experience for Edelman’s London office.
March 27, 2024
|

A New Strategic Vision to Revitalise London’s Fleet Street Quarter
How the Fleet Street Quarter Public Realm Strategy is transforming London’s Central Business District into a vibrant, multimodal Central Social District.
March 26, 2024
|

Three Considerations for Repurposing Stranded Assets for Education
In many instances, abandoned buildings can be converted into thriving schools when they prioritize sustainability, focus on community impact, and offer urban revitalization.
March 25, 2024
|

Trends to Watch: How the Rise of Women’s Professional Sports Is Impacting Venue Design
We talked to six leaders from Gensler’s sports practice about new trends informing the planning and design for the boom in women’s professional sports teams.
March 21, 2024
|

Putting the Patient at the Center of the Health-And-Wellness Equation
Consumer culture, personalized medicine, and technology are extending conversations about well-being far beyond doctors’ offices and hospitals.
March 19, 2024
|

From Canvas to Community: The Art of Placemaking at the Moody Center
Moody Center creates a space where art, culture, and community converge, inviting visitors to become active participants in the placemaking process.
March 13, 2024
|

From Skyline to Shoreline: A Vision for Mixed-Use Spaces in Miami
Miami stands on the brink of an urban renaissance, with the potential to model a visionary urban landscape that champions sustainability, resilience, and vibrancy.
March 13, 2024
|

2024: The Year of the Intentional Workplace
Here are three strategies for leveraging your brand to tame workplace uncertainty.
March 12, 2024
|

Design Is an “Experience Multiplier” for the Built Environment
Sports and entertainment projects are transforming from inward-looking, stand-alone, single-use facilities into multipurpose entertainment districts with 24/7 activation.
March 12, 2024
|

Reimagining Public Space in the Mixed-Use Indian Landscape
As integrated townships in India increase in popularity, we have an opportunity to create functional and resilient public spaces that increase community well-being.
March 08, 2024
|

Now More Than Ever, Quality of Place Matters
Thoughtful, strategic placemaking will ensure successful investments in truly durable places within our cities.
March 07, 2024
|

Using Design to Support Case-Based Learning in Medical Education
At the University of California Irvine, Gensler created an active learning center designed to facilitate a new style of hands-on, experiential learning.
March 06, 2024
|

Ensuring the Future Health of Our Cities
The places we build today will remain standing for generations to come, so they must be able to transform and accommodate new uses as the need arises.
March 05, 2024
|

Gensler Voices: Tobi Sobowale on The Intersection of Art and Design
Tobi Sobowale, a architectural assistant for Gensler London, shares how mentorship can empower and educate.
March 04, 2024

Reframing Design Through the Lens of Restorative Justice
By engaging restorative justice principles from the outset of the design process, we can begin to dismantle inequity in our communities and cities.
February 28, 2024
|

How Tomorrow’s Workforce Will Shape Future Workplace Design
By taking cues from higher education and integrating insights into workplace design, we can create spaces that attract talent and empower tomorrow’s workforce to succeed.
February 27, 2024
|

The Workplace Must Be a Destination, Not an Obligation
The purpose and value of the workplace have never been clearer — and its design has never been more important.
February 27, 2024
|

What About Wednesdays? Planning for the Busiest Day of the Week in the New Hybrid Office.
Learn how organizations can prepare and plan for the busiest day in the hybrid workplace.
February 26, 2024
|

Gensler Voices: Ryley Poblete on His Favorite Gensler Project
Ryley Poblete, a designer for Gensler Los Angeles, shares how mentorship can empower and educate.
February 26, 2024

What Young Associates Want From Modern Law Firms
The legal workplace plays a critical role in retention. Now, more than ever, it must deliver an experience.
February 20, 2024
|

Designing for Ageless Communities
Increased longevity changes not only the way we need to deliver and receive care but also how we think about the future of living, and working.
February 20, 2024
|

Equity and Aging in the 20-Minute City
By designing spaces that prioritize universal design principles and connectivity, we can create more accessible, purposeful places for seniors.
February 15, 2024
|
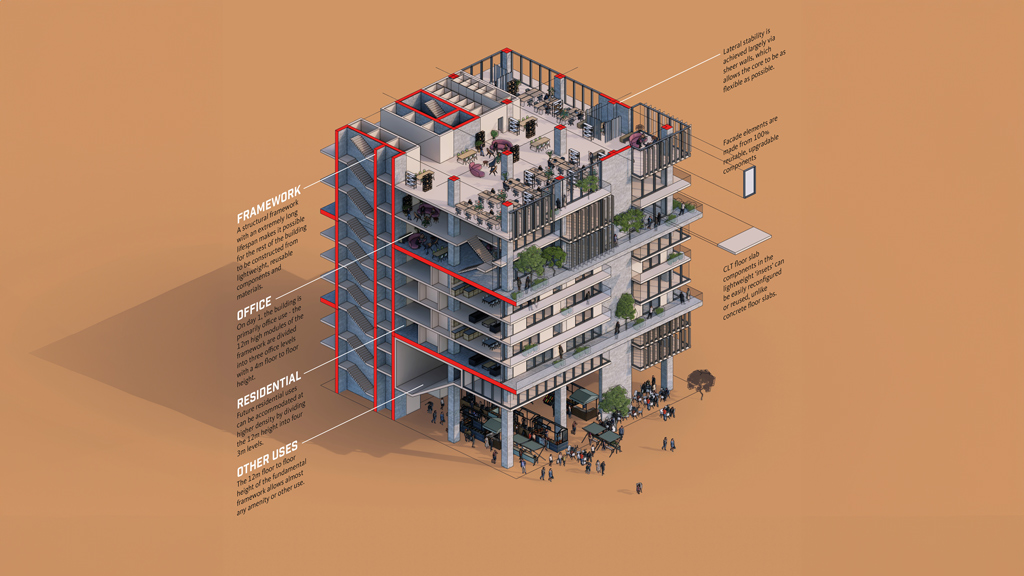
The 600-Year Office
How can we design offices that plan for future uses and adaptations, rather than just the way we work today?
February 14, 2024
|

Toronto’s New Deal Highlights the Importance of Healthy Cities
Here are three areas Toronto can focus on to bring people downtown, improve accessibility, and provide a better central business district experience for all.
February 13, 2024
|

How BMO Stadium Extends the Fan Experience Beyond the Gate
A year-round destination and community asset, BMO Stadium in Los Angeles is a model for other sports and entertainment venues.
February 07, 2024
|

How to Design Practice Facilities Centered on Athletes’ Mental Health
Sports training facilities and performance centers are emphasizing supporting spaces focused on mental health, a key factor in an athlete’s development and overall success.
February 06, 2024
|

Why More Corporate Offices Are Moving to Suburban Downtowns
As more businesses relocate their headquarters to suburban downtowns, the benefits are transformative for companies, employees, and communities.
February 05, 2024
|

New Atlanta Hotel Blends Southern Hospitality and Design Excellence
Signia by Hilton Atlanta pays homage to Atlanta’s rich history while embracing its dynamic present and ever-evolving landscape.
February 05, 2024
|

How Customer Experience Centers Unify Spatial and Digital Branding
A new approach to customer experience center design is helping businesses reimagine customer engagement.
January 31, 2024
|

The Future of Receiving Healthcare at Home
With a new vision for the healthcare landscape, the home will begin to be one of many spaces people can expect to receive high-quality care.
January 29, 2024
|

Severe Weather: The New Design Imperative
Buildings must be designed to protect the health, safety, and welfare of the public — and our infrastructure must be designed to withstand these extreme climatic events.
January 25, 2024
|

Redefining Class A Office Space in Charlotte: A Prototype for Emerging Cities
Through thoughtful repositioning of Class A buildings, emerging cities can create and sustain vibrant, thriving urban centers that attract workers and businesses.
January 23, 2024
|

Thinking Outside the (Big) Box
To elevate former retail shells into inspiring and efficient workplaces, several major considerations must be addressed to achieve successful results.
January 18, 2024
|

Gensler’s New San Francisco Office: A Prototype for the Future of Work
Gensler’s new San Francisco office is a living lab for sustainability and innovation, designed to support new ways of working.
January 17, 2024
|

Defining Active Adult: A Promising Housing Model for an Active Aging Future
Active Adult is a rapidly evolving topic in response to the challenges facing the senior living industry.
January 12, 2024
|

How eVTOLs Could Create a More Inclusive, Sustainable Future for Mobility
Advanced air mobility could have transformative effects on the way we live, creating an inclusive and sustainable future of mobility for all.
January 09, 2024
|

What’s the Recipe for a Great Central Business District?
Honing in on the amenities, activities, transportation options, and experiences that urban residents desire.
January 08, 2024
|

When the Commute Is Worth the Carbon
The Gensler Research Institute has consistently studied the pandemic's impact on work, revealing a persistent concern for organizations and cities: the commute.
January 08, 2024
|

How Life Sciences Developments Can Redefine Urban Areas
Sciences R&D developments are migrating to amenitized urban areas, unlocking opportunity for architectural innovation.
January 08, 2024
|

With a Focus on Sustainability, School Revamp Provides Hope in a Food Desert
Gensler’s Roots to Success initiative at Kelly Miller Middle School is a beacon of hope in a low-income neighborhood in Washington, D.C.
January 02, 2024
|

What We’ve Learned in Three Years Studying Higher Education
As more students return to campus, hybrid and virtual learning are suffering.
December 22, 2023
|

10 Workplace Trends for 2024: What’s In and What’s Out?
To evolve with changing demands and earn people’s commutes, the workplace will undergo key shifts. Here are 10 emerging workplace trends to watch in 2024.
December 20, 2023
|

Rethinking Housing: Innovative Solutions to California’s Homelessness Crisis
DignityMoves Founder and CEO Elizabeth Funk discusses why new thinking is necessary to help solve the housing and homelessness crisis.
December 18, 2023

Open or Private? It’s Time for a New Workplace Model.
The debate of open versus private workspace has resurfaced. But today we work differently, it’s time for a new workplace model.
December 14, 2023
|

The Trends Shaping the Future of Hospitality
What are the biggest trends impacting hospitality operators? Gensler’s global hospitality leaders discuss what’s next for hospitality design.
December 13, 2023
|

Blowing the Lid Off Product Design:
5 Tips for a Better Trash Receptacle
When it comes to commercial grade trash receptacles, there’s no shortage of ways to throw things out, but many available options still fall short of addressing clients' needs.
December 13, 2023
|

Trends to Watch: Shaping the Future of Higher Education
With institutions facing challenges such as declining enrollment and rising costs, Gensler’s Education leaders discuss what’s next for the future of higher education.
December 07, 2023
|

COP28 Day 3 Recap: Designing for a More Resilient Future
One key theme to emerge from our conversations at COP28 in Dubai is the need to create a culture of sustainability in every project we take on and every space we design.
December 06, 2023
|

COP28 Day 2 Recap: Leading the Way to Smarter, Greener Cities
Our industry must continue to push the pace of innovation to deliver affordable solutions for today’s challenges. Read more insights from our second day at COP28.
December 05, 2023
|

COP28 Day 1 Recap: Decarbonizing the Built Environment Is a Global Priority
By putting our energy toward decarbonizing the built environment, we are investing in that future. Here are some key takeaways from COP28.
December 04, 2023
|

Trends to Watch: How Developers Can Make Buildings More Adaptable, Relevant, and Resilient
Gensler’s Office Developers leaders discuss how to make office buildings more relevant, sustainable, and resilient to increase long-term value.
December 01, 2023
|

Rethinking Law Firm Workplaces in the Age of Hybrid Work
The law office of the future will be a place where lawyers will learn to work differently, supported by innovative design and technology.
November 30, 2023
|

Feng Shui Meets Sustainability: 5 Ideas for a Greener Future
Here are five ideas exploring the intersection of Feng Shui and sustainability in the built environment.
November 29, 2023
|

Office-to-Everything: A New Path for Revitalizing Downtowns
In the local New York City market, there is huge potential to return stranded assets back to their highest and best use by embracing diverse conversion types.
November 27, 2023
|

Ecological Urbanism Is the Future for Cities in the GCC
As more people move to urban areas, it is essential that our urban spaces be designed in a more ecological manner.
November 27, 2023
|

Unlocking the Value of ESG
Buildings that can show environmental responsibility and positive impacts in our community will have a competitive advantage among tenants and investors.
November 21, 2023
|

Retail Design for Better Consumer and Employee Experiences
The recent resurgence of in-person retail brings with it not only a new consumer experience, but an equal emphasis on a new employee experience.
November 17, 2023
|

Leading With Values Is Key to Engaging Next-Gen Workers
As Gen Z enters the workforce, companies that lead with values, using space as a vehicle to amplify connections, will have a competitive edge.
November 16, 2023
|

10 Considerations for Transitioning Back to Work in a Hybrid World
Here are 10 considerations, tools, and methodologies for creating a better workplace experience and attracting people back to the office in a hybrid world.
November 16, 2023
|

Verbal Identity Is Key to More Inclusive Brand Storytelling
Verbal identity will play an increasingly important role in creating brand expressions that equalize and diversify brand experience for everyone.
November 15, 2023
|

Gensler Voices: Brian Hunt on How Sports Have Influenced His Design Career
Brian Hunt, a designer for Gensler Chicago, shares what’s influenced his design career and advice for those beginning their career.
November 15, 2023

As Streaming Accelerates, New Jersey Is Open for Business
With its wide array of resources and existing infrastructure, New Jersey is emerging as a competitive market for studio and soundstage spaces.
November 15, 2023
|

The Climate Crisis Is Also a Well-Being Crisis
Climate change is emerging as a profound global concern and appears to have an outsize impact on the mental health and well-being of younger generations.
November 14, 2023
|

Immersive Experiences: A Movement Beyond Fad
In the rapidly evolving technology landscape in the built environment, immersive digital experiences are not a fleeting fad; they have become an expectation.
November 14, 2023
|

What Makes a Great Retail Experience? Community, Connection, and Exhibition
Astute retail and hospitality brands recognize that in-person connection is a vital part of their offerings. But what does that visceral experience actually look like?
November 10, 2023
|

Using Experience Strategy to Design What People Truly Want
By vividly depicting potential users early in the design process, the resulting room, building, or campus is more likely to meet their needs.
November 10, 2023
|

Elevating the Retail Experience: 4 Lessons From Airport Lounge Design
Here are four design insights from airport lounge environments that retailers can use to elevate retail consumer environments and experiences.
November 10, 2023
|

Trends Shaping the Integrated Workplace Ecosystem in China
In China, design trends are trending towards workplace campuses that balance operational effectiveness, ample amenities, and carbon consciousness.
November 09, 2023
|

Gensler Voices: Courtney Albracht on Shaping the Future
Courtney Albracht a designer for Gensler Minneapolis, shares how design can impact communities and practitioners alike.
November 08, 2023

As New Work Patterns Emerge, the Workplace Must Respond
Gensler’s exploratory survey of office workers in six U.S. cities aims to better understand how emerging factors impact how and why employees use the office.
November 06, 2023
|

The Future of Central Business Districts Depends on More Than Office Buildings
Gensler’s latest City Pulse reveals how downtowns can adapt to a changing world — and deliver great experiences.
October 31, 2023
|

Second Summer: Adaptable Shading Solutions for Unpredictable Seasons
Continuing to rely on energy-intensive solutions to manage excessive heat will result in a cascading impact on carbon emissions. We need passive, adaptable solutions.
October 31, 2023
|

Amenities at the Edge: Where the Workplace Meets the Street
We have an opportunity to reimagine the ground floor of our cities — reinventing sidewalk-facing storefronts to serve the community, not just the daytime workforce.
October 31, 2023
|

AI and the Future of Smart(er) Cities
Our recent work is starting to bring into focus some shared characteristics and design principles for urban-scale technology and AI.
October 30, 2023
|

Why We Need Bold Change to Revitalize Our Cities
While there are points of concern for the current state of our city centers, this is also a unique opportunity to create meaningful and lasting change.
October 27, 2023
|

Gensler Voices: Dena Wangberg on Her Start in Architecture and Design
Dena Wangberg, designer for Gensler Raleigh, chats about her first foray into architecture and design and the power of a mentor.
October 25, 2023

Dear Downtown, Let’s Rewrite Our Story
How can our cities serve our deepest need — the need for belonging and connection with each other? We have to write a new story.
October 25, 2023
|

Designing a New Workplace to Embrace Future Workstyles
The new workplace experience must be elevated to embrace new workstyles.
October 24, 2023
|

What We’ve Learned by Assessing More Than 1,300 Potential Office-to-Residential Conversions
We’ve developed a process for evaluating existing office buildings to determine if they are candidates for multifamily residential conversions.
October 23, 2023
|

The Definitive Value of Build to Suit: Building Purpose From the Ground Up
These purpose-built office buildings or headquarters can be developed to suit a company’s specific needs and reflect its unique brand and culture.
October 23, 2023
|

Embodied Carbon Is Where Tech Must Tighten Its Belt
As buildings get more efficient and power grids get cleaner, projects are looking to where they can further reduce their carbon footprint to meet their net zero commitments.
October 18, 2023
|

Purpose of Place: Why Place Branding Matters
Place branding can shape people’s perceptions about that place and drive its competitive identity.
October 17, 2023
|

Gensler Voices: Shane Mathewson on the Ever Evolving Gensler Experience
Shane Mathewson, a designer for Gensler Chicago, chats about the web of influence that helps grow design talent.
October 16, 2023

4 Ways AI Can Create a More Engaging and Enriching Workplace Experience
Here are four considerations that can help designers and organizations use artificial intelligence to create a more engaging and enriching workplace experience.
October 11, 2023
|

The Benefits of Repurposing Stranded Assets as First-Generation Labs
As we consider the possibilities of conversions for stranded assets, it’s important to identify laboratories as a potential use.
October 10, 2023
|

Gensler Voices: Evan Ahn on the Prioritization of Space
Evan Ahn, a designer for Gensler Detroit, chats about the “why” when designing a space.
October 09, 2023

Fast.Forward.: A New Model for Academic Science Facilities
We created a data-powered concept for how academic science facilities of the future will perform, feel, and look.
October 09, 2023
|

Adapting Big Box Retail Stores to Healthcare Clinics
Transforming abandoned storefronts into dynamic healthcare clinics can be a cost-effective and efficient way to deliver medical services to communities.
October 09, 2023
|

How Union Square Can Become San Francisco’s New Central Social District
We outline five ideas for transforming San Francisco’s Union Square into a dynamic, 24/7 destination.
October 05, 2023
|

Gensler Voices: Gabriela Alvergue on The Skills To Succeed in Design
Gabriela Alvergue, a designer for Gensler Chicago, shares her career journey in design from early influences to her favorite projects.
October 04, 2023

A Viable Future for L.A. Starts With Public-Private Partnerships
By partnering with the private sector, the City of L.A. can avoid a downward spiral of disinvestment and flight from Downtown L.A.
October 04, 2023
|
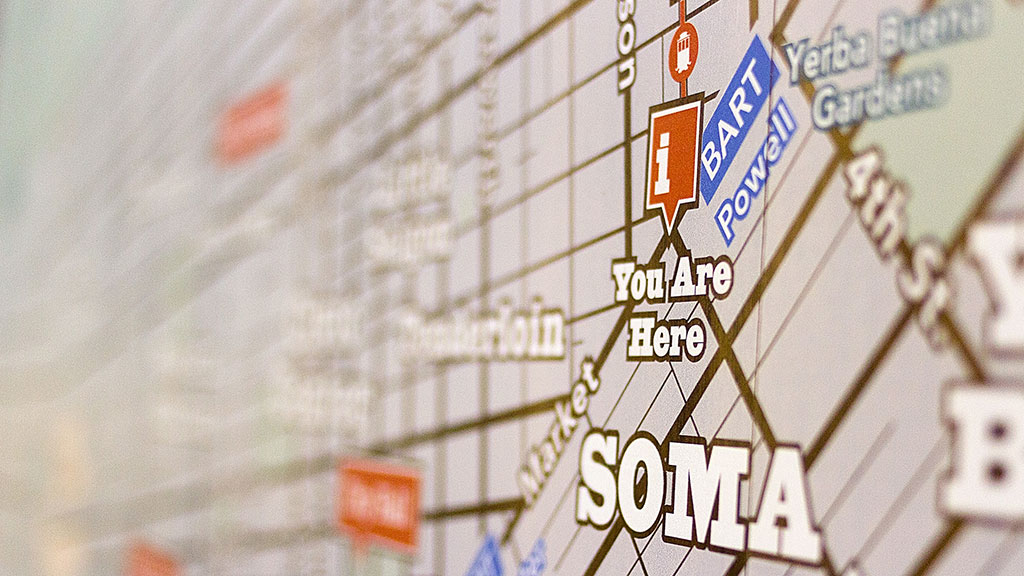
Why Cities Like San Francisco Need More Place Positivity
As San Francisco city advocates try to counter a wave of negative sentiment, how can they share residents’ own experience and sense of community in an authentic way?
October 03, 2023
|

Extreme Weather Demands an Immediate Design Response
Gensler’s Climate Action Survey 2023 explores how design can address the rapidly accelerating climate crisis.
October 02, 2023
|

The Law Firm of the Future: Can a Workplace be Restorative?
Over the past year, we've taken a deep dive into the measurable impacts facing professional service firms and how these impacts are affecting the current legal workplace.
September 29, 2023
|

How Changing Traveler Demands Are Reshaping Hospitality
Consumers are demanding more from their travel experiences. Here’s how hospitality can respond.
September 29, 2023
|

Gensler Voices: Veterans at Gensler Discuss Leadership, Trust, and Their Military Experiences
We sat down with United States military veterans to explore how the military has informed and inspired their work at Gensler.
September 25, 2023

Pilots in Practice: Key Insights Shaping the Future of Work
We’ve outlined strategies and considerations for executing a successful workplace pilot.
September 21, 2023
|

The Studio Lab: An Experimental Approach to Transform the Workplace
Across industries, organizations are rethinking ways to engage their employees and create thriving workplaces. We introduce The Studio Lab.
September 20, 2023
|

How Your Workplace Can Maximise Trust — and Why It Matters
Trust is foundational to doing good work and building strong professional teams. What if the workplace becomes the cornerstone of an emergent economy based upon trust?
September 19, 2023
|

Gensler Voices: Katie Karlinchak on the Impact of Universal Design
Katie Karlinchak, a designer for Gensler San Diego, chats about how early influences from family members jumpstarted her design career.
September 19, 2023

Strategies for Reinvigorating Singapore’s Central Business District
Placemaking strategies can provide attractive Central Business Districts that encourage workers to return to the workplace.
September 18, 2023
|

5 Strategies for Heat Resilient Design
Here are five strategies we need to embrace to create heat resilient design solutions for the coming years.
September 15, 2023
|

What Airports Can Learn From Work, Sports, Healthcare, and Retail
Here are five cues that airports can take from innovations, insights, and perspectives from other parallel industries.
September 13, 2023
|

The EV Revolution — And Why Charging Stations Are So Critical
Gensler’s mobility and aviation experts discuss what’s next for electric vehicles, EV charging stations, and more.
September 13, 2023
|

Gensler Voices: Nick Acevedo on Transformation
Nick Acevedo, a designer for Gensler Newport Beach, chats about the benefits of learning throughout your design career.
September 13, 2023
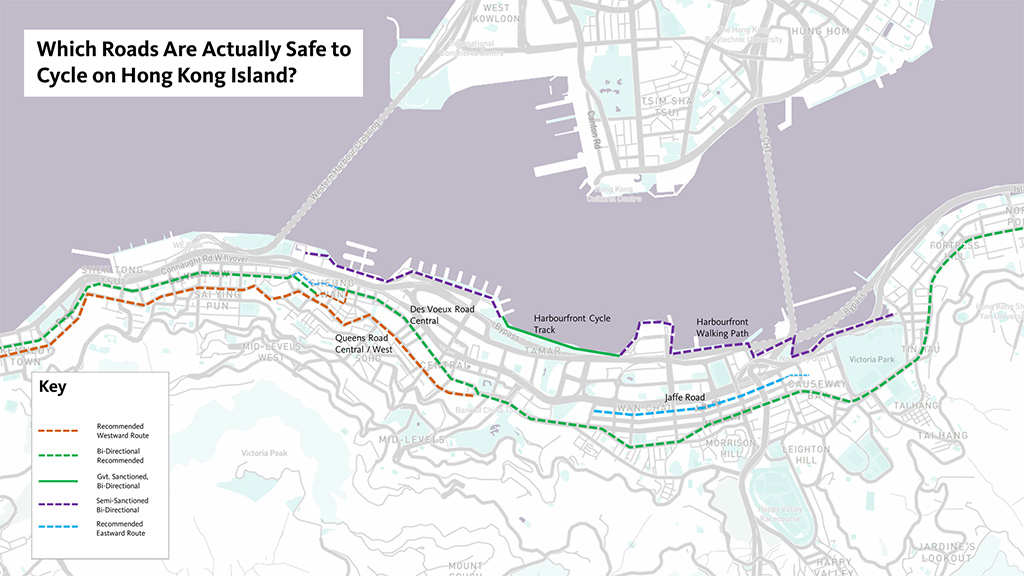
Commuting by Bicycle in One of the Most Cycling-Unfriendly Cities
Is there opportunity for micromobility in Hong Kong? A look at cycling in Hong Kong’s CBD.
September 13, 2023
|

Understanding the Modern Transit Passenger Experience
What makes a great (or not-so-great) transit experience? Here are five factors that drive passenger experience.
September 11, 2023
|

Gensler Voices: Gabby McCloy on the Learning Curve to Growth
Gabby McCloy, a designer for Gensler Raleigh, chats about entering the design workforce and what emerging and growing trends in the industry are most exciting.
September 08, 2023

Fixed Base Operators: A Gateway to eVTOL Takeoff
The Advanced Air Mobility (AAM) and electric Vertical Takeoff and Landing (eVTOL) revolution is already here. See how eVTOL is taking off.
September 07, 2023
|

Borealis: The Opportunity for Building Integrated Carbon Capture to Reverse the Carbon Footprint of Buildings
If applied across Gensler’s global portfolio, direct air capture technologies could remove 14.5 million tonnes of CO2 from the atmosphere.
September 06, 2023
|

Micro-Fulfillment: The Next Step to Faster, More Efficient Last-Mile Delivery
As more people shop online, micro-fulfillment strategies can improve delivery times. Here are five considerations to meet the challenges of last-mile delivery.
September 05, 2023
|

The Impact of Artificial Intelligence on Data Center Design
The increased demands on data centers to perform AI computing is driving architects, engineers, and owners to find innovative design solutions.
September 01, 2023
|

The Benefits of Nurturing Organizational Pride in Life Science Workplaces
In our latest survey of research scientists, we uncovered how laboratory design can promote a sense of organizational pride.
August 30, 2023
|

Designing for the Convergence of Science at The Engine
MIT’s The Engine enables scientists, engineers, academics, and business leaders to collaborate under one roof.
August 30, 2023
|

How Business Schools Fuel Innovation Ecosystems
By creating highly connective business school “ecosystems,” there is significant untapped potential to help cities and communities thrive.
August 29, 2023
|

5 Strategies for Labs to Meet ESG Targets
These key strategies can achieve significant reductions in a laboratory tenant’s carbon footprint.
August 28, 2023
|

The Future of Healthcare as an Integrated Ecosystem of Health and Care
By refocusing the U.S. health system on improving community health, we can provide better outcomes and address the industry's major challenges.
August 23, 2023
|

What Two Leading Edge Venues Reveal About the Future of College Sports
Sports venues must go beyond game day and do more for the team, the campus community, and the general public by identifying year-round use.
August 22, 2023
|

How the EveryFan Journey Drives Engagement in Stadium Design
Today’s sports and entertainment venue experience is no longer solely about the event itself; it is intrinsically connected to the fan journey.
August 22, 2023
|

A Material Approach to Lowering Carbon and Changing the Building Industry
Gensler Co-CEO Jordan Goldstein talks about Gensler’s Product Sustainability (GPS) Standards and what it means for the industry.
August 21, 2023
|

Driving Transformational Change in Denver Through Human-Centered Design
A conversation with Gensler Denver’s Co-Managing Directors Michelle Liebling and Jon Gambrill.
August 15, 2023
|

How Augmented Reality Can Drive More Engaged Communities
New and emerging technologies are bringing even more opportunity to enhance the ways communities engage with the cities around them.
August 14, 2023
|

Why Biophilic Design Is Crucial in the Workplace and Beyond
Good biophilic design celebrates our love of life to create spaces that inspire, empower, and energise the people who use them.
August 09, 2023
|

Introducing the Club Workplace
A neighborhood workplace that combines the work-oriented spaces of a Hub office with the convenience of a reduced commute.
August 08, 2023
|

The Future of Sports Venues Is About Creating Vibrant, Multiuse Districts
Gensler’s Director of Sports explains why integrating sports venues into the urban fabric can generate revenue and create live-work-play communities.
August 01, 2023
|
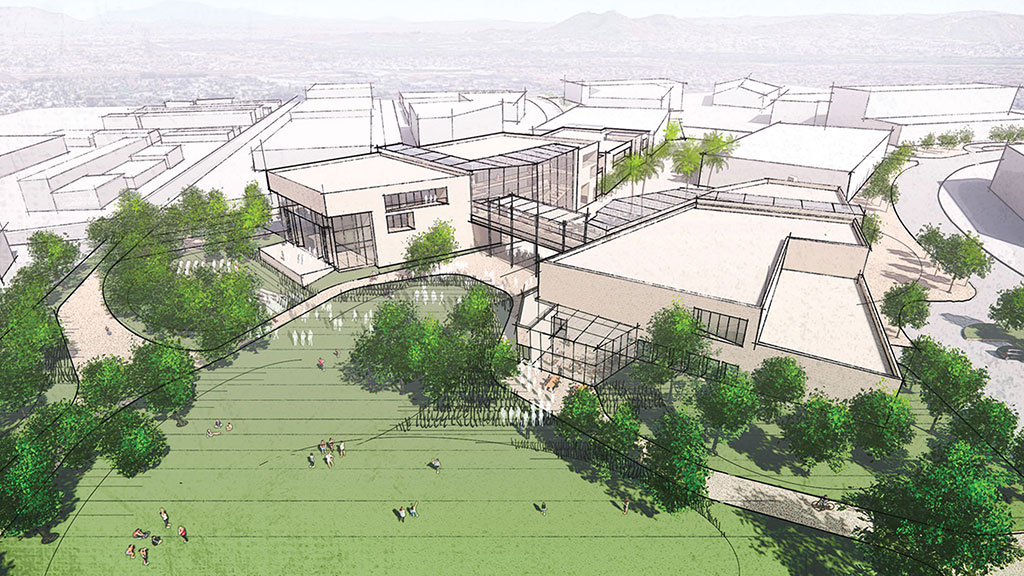
How Civic Architecture Can Strengthen Our Social Fabric
The design of our civic buildings and public spaces can influence our personal and societal health.
July 27, 2023
|

Fans Are Hungry for New Seating Options at Sports Venues
The “one ticket, one seat” model has run its course. From standing only to sponsored zones, a full menu of ticket types is needed to meet consumer demand for live sports.
July 27, 2023
|

How to Reposition Office Space for Market Differentiation
We must shift our thinking to focus less on workplace density and more on the experience and quality of space the office can deliver.
July 25, 2023
|

Resuscitating Buildings for Life Sciences and Healthcare
By reusing existing buildings, such as empty retail stores and office buildings, architects can bring health, sciences, and wellness services closer to communities.
July 19, 2023
|

From Pilots to Policy: Exploring Office-to-Residential Conversions in Boston
There are clear steps that can be taken to address the housing shortage, and we believe there is huge opportunity in office-to-residential conversion.
July 19, 2023
|

People Have Choice in the Workplace, But Not the Choices They Need
Providing greater choice in where to work within the work environment doesn’t just enhance the workplace experience; it can lead to better business performance.
July 18, 2023
|

Designing Empathetic Workplaces Can Be a Key Differentiator
Empathy is a required trait of healthy workplaces and communities, and a key differentiator.
July 17, 2023
|
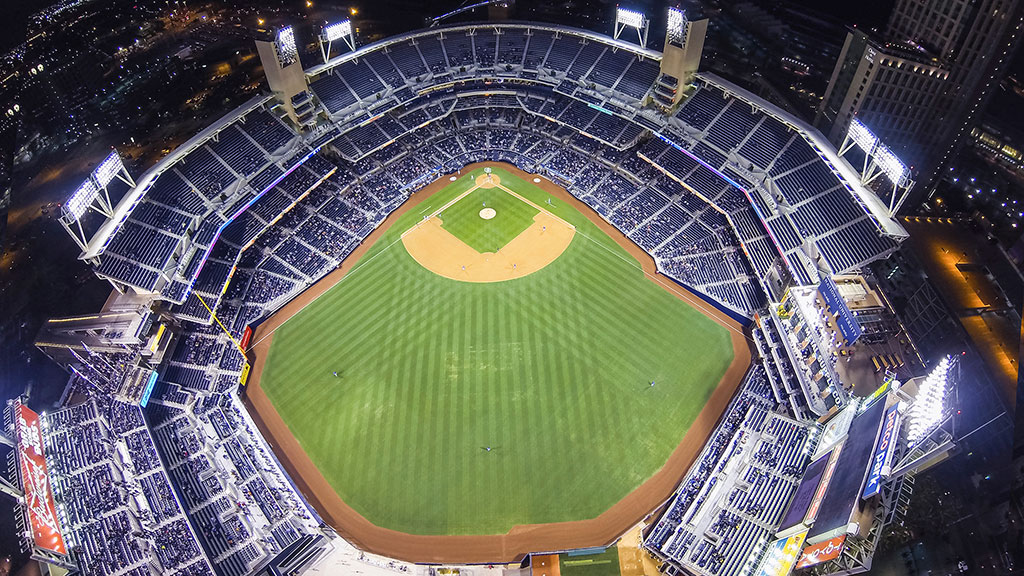
Baseball Is Changing. Here’s How Cities Could Change With It.
As the future of downtowns evolves and baseball continues to grow, here are five ideas for how ballparks and urban districts could improve.
July 14, 2023
|

High-Performing Workplaces Spark Employees’ Intrinsic Motivation
By tapping into employees’ intrinsic motivation in the workplace, employers can drive business results.
July 13, 2023
|

5 Trends Driving the New Workplace
Here are five workplace trends that have been accelerated and now are driving priorities for the office of the future.
July 12, 2023
|

The Future of Work in Canada: Insights From Gensler’s Global Workplace Survey
Gensler’s latest global workplace survey reveals that Canadian offices are ripe for post-pandemic reinvention.
July 10, 2023
|

Reinventing the Airport as an All-in-One Facility
Can an airport simultaneously be a great international gateway, a thriving community asset, and an efficient transfer hub?
July 05, 2023
|

Evolution of the Legal Workplace
To bring people back to the office, law firms and other high-performing companies need to intentionally plan their workplaces for collaboration, productivity, and culture.
July 05, 2023
|

The UnOffice: Workplaces for More Than Productivity
The next evolution of the workplace should be designed for hybrid work, embracing both productivity and unproductivity.
June 29, 2023
|

Why Airports Must Create a ‘Place of Sense’ to Engage Travelers
To transform a passenger’s journey from good to great, we believe the only way to create a sense of place is to first create a “place of sense.”
June 28, 2023
|

AI Is Already Changing Hospitality. Here’s How.
From optimizing energy efficiency to hotel operations, AI is revolutionizing the hospitality industry in ways that are delightful and profound.
June 26, 2023
|

To Foster an Engaged Student Body, Holistic Campus Design Is Key
To address declining enrollment and changing student expectations, higher education campus design should strive to build an engaged community.
June 22, 2023
|

Beyond Books, Libraries Are Vital Community Hubs
Beyond their traditional role as information providers, municipal libraries are uniquely positioned to have a positive impact on the communities they serve.
June 21, 2023
|

SHED: Connecting the Dots Between Education, Industry, and Technology
Blurring traditional boundaries between sciences will foster curiosity and exploration in new and emerging disciplines.
June 20, 2023
|

Why Connected Neighborhoods Are Key to Urban Revitalization
In cities like Nashville, new development must consider the need to enhance neighborhood character and a connected urban experience.
June 19, 2023
|

5 Ways Educational Anchor Institutions Can Catalyze Economic Recovery
As post-pandemic cities struggle to rebound, educational anchor institutions can be an important player in helping local economies recover.
June 16, 2023
|

Why It’s Time to Reframe the Conversation Around Senior Living
New Gensler research demystifies myths about aging and offers creative solutions for communities that are currently not built to support older people.
June 15, 2023
|

Why Designing for the Human Experience Is Key to Advancing SDG Goals
In times of radical change and crisis, we can leverage design for positive impact. Design is pivotal to achieving sustainable development goals.
June 14, 2023
|

Hybrid Is Here to Stay. So Is the Office.
Gensler’s global workplace research reveals an optimistic future: while hybrid work is here to stay, the office is needed more than ever.
June 13, 2023
|

Transforming a Generational Asset Into a Class A Tower
The reinvestment in 633 Folsom transformed a 1960s asset to reduce carbon and reanimate a vital urban corridor.
June 08, 2023
|

Bring Climate Justice Into Your Projects by Engaging Community Partners
Our cities are full of organizations that are well-equipped with amazing expertise and can help guide projects to have long-lasting impact.
June 07, 2023
|

Gensler Voices: Argelia Bárcena on Serendipitous Moments with Lasting Impact
We sat down with Argelia Bárcena, from our Gensler San Francisco office, to discuss what's ahead for architecture and design and the power of pivoting in your career.
June 06, 2023

Equity and the 20-Minute Neighborhood
To build stronger, more resilient, and equitable communities it’s essential that we leverage the power of research and engage residents.
June 05, 2023
|

5 Trends Changing the Shape of Healthcare Design
The way we deliver and receive care is changing. Here, one of Gensler's healthcare leaders shares her thoughts on five trends currently influencing design in the industry.
June 01, 2023
|

Why It’s Time to Apply Regenerative Systems Design on a Global Scale
Regenerative architecture offers a more sustainable path forward.
May 31, 2023
|

Implementing Science Research Lab Design Strategies in Wineries
Similar to a research lab, wineries and winemakers require a space for analysis and discovery that balances equipment requirements with human-centric design.
May 31, 2023
|

Trends to Watch: The Evolution of the Sciences Workplace
In the Puget Sound region and beyond, the science industry is growing in our post-pandemic economy.
May 30, 2023
|

Supporting Health, Well-Being, and Safety Through Trauma-Informed Design
We’ve outlined seven strategies that any project can implement to support recovery.
May 26, 2023
|

5 Conversations That Define 2023’s Evolving Workplace
Here are five design trends emerging as key drivers for the future workplace.
May 25, 2023
|

Will Third Places Be the Future of Workplaces?
Just like third places, the time has come for the office to open up to the city, the neighbourhood, and the public space, rather than withdrawing into itself.
May 24, 2023
|

Data Centres and the Forgotten Landscapes of Digital Infrastructure
Through regenerative design, we can change the perception of data centres from ‘bad neighbour’ developments to community assets.
May 24, 2023
|

Rethinking Engagement: Strategies for Immersive Design
How can we drive and sustain meaningful engagement between our clients’ spaces and their employees, partners, and customers? Immersive experiences are key.
May 23, 2023
|

Why Brand Fleets Are Key to Creating an Engaging, Multiplatform Experience
Brand fleets can create brand loyalty and reach the customer of now and the younger audience of the future.
May 22, 2023
|
Interactive Graphic: Public Transit Systems Around the World
Survey respondents rated their satisfaction with aspects of public transit systems across cities and identified drivers of a great public transit experience.
May 22, 2023

Younger Generations Work Differently. What Does This Mean for the Future Workplace?
It is crucial to understand generational differences to support a productive and engaged workforce.
May 17, 2023
|

3 Ways the Most Innovative Companies Work Differently
As office workers are returning to the office, we wanted to know: do Innovators work differently, and do they value the office differently?
May 17, 2023
|

What’s Next for Hospitality and New Luxury in Latin America
As a region steeped in culture, history, and beauty, Latin America is a natural fit for the more meaningful experiences that today’s travelers are searching for.
May 16, 2023
|

Checking In on the Guest Experience
As leisure travel ramps up, hotels must do more to exceed guest expectations. Gensler’s Hospitality Experience Survey 2023 sheds light on traveler preferences and behaviors.
May 16, 2023
|

The Future of Hospitality Is Local
Here’s why embracing local cultures and communities is key to creating an authentic hospitality experience.
May 15, 2023
|

How the Renovation of a Landmark Hotel Sets a New Benchmark for Sustainable Design
The renovation of Amway Grand Plaza Hotel Tower demonstrates how holistic improvements can improve a building’s performance and impact carbon emissions.
May 15, 2023
|

The Future of Retail Health and the New Healthcare Experience
Retail health is emerging as a means for delivering quality, convenient care and a model for healthcare systems expanding their networks or services to reach new patients.
May 12, 2023
|

The Future of City Centres
The pandemic has prompted a rethink of the role our city centres as they become more of a lifestyle location rather than a traditional work destination.
May 09, 2023
|

Gensler Voices: Joan Megan Ng on the Beauty of Design
We sat down with Joan Megan Ng, from our Gensler Singapore office, to explore what it’s like to be a project accountant at Gensler.
May 09, 2023

Old to Bold: How Hotel Adaptive Reuse Transforms Communities
Adaptive reuse has become a key strategy for revitalizing economically obsolete structures and breathing new life into urban centers.
May 08, 2023
|

Implementing Sustainable Design Strategies in the Retail Environment
Here’s how linking sustainability efforts to the customer experience helps grow brand value and move us toward a more sustainable future.
May 05, 2023
|
Gensler Voices: Haruka Yokokawa on the Importance of Having a Mission
We sat down with Haruka Yokokawa, from our Gensler Tokyo office, to explore the power of opportunity and learning in your career.
May 03, 2023

What Gensler’s Middle East Workplace Survey Uncovers About How to Attract Talent Back to the Office
Gensler’s Middle East Workplace Survey 2023 examines three ways organizations can attract workers to return to the office.
May 02, 2023
|

Book Depository Jump-Starts Ford’s Detroit Innovation District
As Ford continues to evolve its business for a new century, the company has returned to its roots in the Motor City.
May 02, 2023
|

3 Key Ingredients to Creating a Competitive Advantage in the Future of Work
Why HR, Corporate Real Estate, and Brand need to come together to help companies build a thriving workplace.
May 02, 2023
|

Using Resilient Materials to Make Your Brand Values Tangible
Resilient materials offer an opportunity to tell more rich and meaningful brand stories that offer a vision for an alternative future.
April 27, 2023
|

The Biogenic Materials Revolution Has Begun and Mass Timber Is Leading the Way
Biogenic materials will be crucial in our efforts to address climate change while also meeting the vast global demand for new buildings and spaces.
April 26, 2023
|

How Biophilia, Biomimicry, and Bioclimatic Strategies Will Transform the Future of Design
By incorporating biophilic, bioclimatic, and biomimicry design strategies, we can raise the bar for what acting sustainably means.
April 25, 2023
|

Achieving LEED Zero Energy With HARC
Data-driven sustainability tactics qualified HARC headquarters to become the first LEED Zero Energy Certified commercial building in Texas.
April 25, 2023
|

Climate Change Is Here. It’s Time to Invest in Our Collective Future.
Data from Gensler’s climate change survey offers insights into how climate change is dramatically affecting the international community.
April 20, 2023
|

Back to Basics: 5 Strategies to Approach Net Zero Energy
Tenants are demanding healthy, energy-efficient buildings with measurable data to support ESG and talent retention goals. Here are five strategies to approach net zero energy.
April 19, 2023
|

Why New Construction Cannot Solve the Climate Crisis
To meet carbon reduction goals, why focus on new construction when we can achieve measurable impact by focusing on existing building renovations?
April 18, 2023
|

Mass Timber: The Sustainable Solution for the Design Industry (Part 2)
In this episode of the Gensler Design Exchange podcast, we continue a conversation around mass timber.
April 17, 2023

An Evolving Practice: Industrial Architecture
Today, we are seeing production and logistics facilities pop-up closer to, and even within, our cities and communities.
April 14, 2023
|

Trends to Watch: What’s Next for Media Workplaces?
Here are four factors driving the future of media workplaces and their unique set of needs.
April 13, 2023
|

Adobe’s Founders Tower Provides a Glimpse Into the Future of Work
Adobe’s Founders Tower embodies the company’s commitment to creativity, sustainability, inclusivity, and an innovative approach to the future of work.
April 12, 2023
|

A Living Lab: How the Gensler Phoenix Redesign Supports Our New Work Styles
At the beginning of 2020, the Gensler Phoenix office set out to design a workplace model that would support flexibility for seamless collaboration and innovation.
April 12, 2023
|

What It Means to Be a “Healthy Building”
Healthy buildings have a direct impact on our ability to thrive. Here are some strategies for future projects seeking to emphasize health and well-being.
April 11, 2023
|

Gensler Voices: Jacob Simons on the Power of Community
We sat down with Jacob Simons, Northwest Regional Strategy Practice Leader in our Gensler Seattle office, to discuss the power in leaving a legacy of positivity.
April 11, 2023

Mass Timber: The Sustainable Solution for the Design Industry
In this episode of the Gensler Design Exchange podcast, our guests discuss what mass timber is, where it comes from, and why we should be using a lot more of it.
April 07, 2023

Trends to Watch: Shaping the Future of Attainable Housing
Gensler Residential Leader Kelly Farrell discusses attainable housing trends and potential solutions.
April 05, 2023

Thinking Outside the Wooden Box: An Alternate Construction Method for Resilient Affordable Housing
Thin-shell concrete construction has just recently begun to establish a foothold in the United States, but has been used globally for years.
April 05, 2023
|

Gensler Voices: Nupur Shah on Defying Expectations
We sat down with Nupur Shah, senior designer, Gensler Bangalore, to ask her about how her unconventional career shift from healthcare to design has guided her work.
April 04, 2023

Product Design for a
Better Bathroom Experience
Gensler’s product designers reimagined stainless steel bathroom accessories to deliver a better, more inclusive bathroom experience.
April 03, 2023
|

What Is the Architect’s Role in Creating Equitable Communities?
In this episode of Gensler Design Exchange podcast, our guests talk about this new resource for architects and designers in creating equitable communities.
March 30, 2023

Trends to Watch: 5 Opportunities Shaping the Future of Tech in the Built Environment
Here are five opportunities that shape the future of technology in the built environment.
March 29, 2023
|
The Internet of Places: How Will Web3 Transform the Built Environment?
See how new tech trends in AI, VR, and Web3 will transform the built environment.
March 29, 2023
|

The Bon Brings A New Model for Urban Living to Boston
Adjacent to mass transit in the heart of Boston’s Fenway neighborhood, the Bon’s shared amenities and unique ground floor program create a new kind of community.
March 28, 2023
|

Gensler Voices: Mohammed Mushaikh on Perseverance in Pursuit of Your Goals
We asked Mohammed Mushaikh, a designer in Gensler’s Riyadh office, to reflect on how architecture and design can drive equitability and inclusivity in our communities.
March 28, 2023

(Re)Shaping the Future of Financial Services Firms in London
Here are three meta trends that will continue to shape the financial services workplace and drive change for business and corporate real estate.
March 23, 2023
|

What Gensler’s Mexico Workplace Survey Reveals About Why Employees Are Returning to the Office
Gensler’s Mexico Workplace Survey uncover which spaces and experiences are most effective in supporting employees.
March 22, 2023
|

Gensler Voices: Lina Ayala on the Power of Mentorship in Her Career
Lina Ayala, residential practice area office leader for Gensler Sydney, chats about the role that her mentor and international opportunities have had on her career.
March 21, 2023

Future-Prepping Your Business in an Uncertain World
Our world is full of unknowns. What can we do about it? “Futures” (or future-casting) are another way to think about and plan for what might be coming next.
March 20, 2023
|

Gensler Voices: Dijana Dejanovic on the Importance of Inclusivity in Strengthening Design
We sat down with Dijana Dejanovic, from our Gensler London office, to discuss the future of architecture and design and how diverse backgrounds elevate the design experience.
March 16, 2023
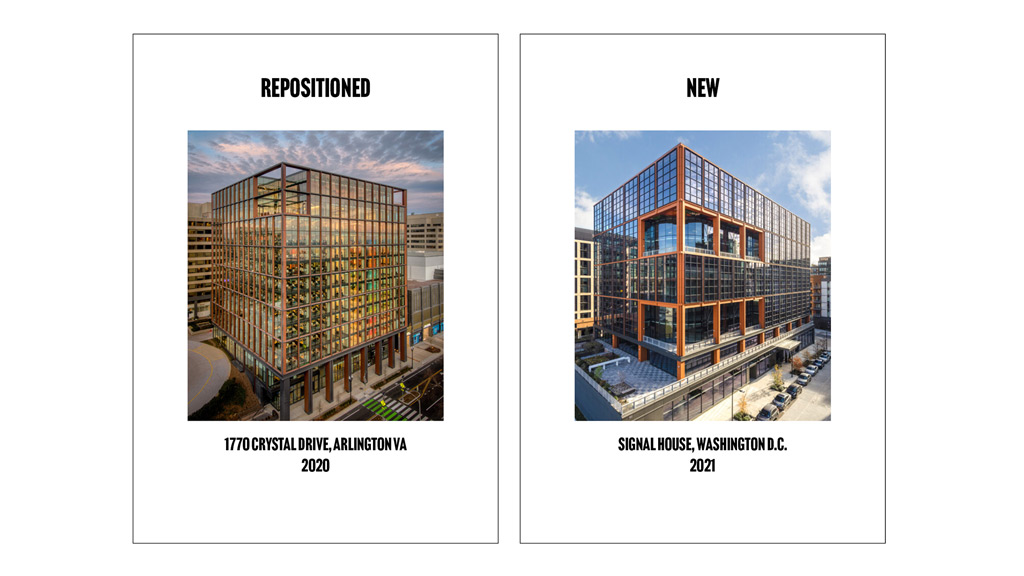
Does Your Old Building Have More Potential Than You Think?
By optimizing the strong foundation of older assets with strategic design interventions, existing office buildings may have more transformative potential than expected.
March 15, 2023
|

Listening vs. Prescribing: Understanding How Students Perceive Education Spaces Today
To design schools where students feel like they truly belong, it is critical to hear directly from the students about their lived experiences.
March 13, 2023
|

Designing Innovative Pathways to Affordable Housing in Los Angeles
Gensler’s Roger Sherman discusses affordable housing pathways, multigenerational living, co-living solutions, and more.
March 10, 2023
|

The Future of Travel? Start With the Future Traveler.
To be truly inclusive, airports must address a diversity of passenger and employee needs.
March 09, 2023
|

Trends to Watch Shaping the Future of Urban Mobility
Gensler’s research, planning, and transportation experts discuss how residents’ mobility experiences, opinions, and preferences are shaping how cities are planned and built.
March 07, 2023

Libraries Are Crucial Social Infrastructure for the 20-Minute City
Once known solely as places for books, libraries are pivoting and adapting to adopt new roles in society.
March 03, 2023
|

An Opportunity to Unlock Value for Underutilized Assets: Office Conversions for Senior Living
In the race to convert vacant office buildings, developers should consider senior living.
March 01, 2023
|

Housing Affordability and Homelessness in Los Angeles: A Conversation With Roger Sherman
Gensler’s Roger Sherman discusses housing affordability, homelessness, and innovative solutions for reform.
February 28, 2023

What Gensler’s Canadian Workplace Survey Reveals About the New Priorities for Office Design
Gensler's Canada Workplace Survey 2022 survey finds that the office will remain a critical part of the work ecosystem, but there are some challenges.
February 23, 2023
|

3 Leadership Disconnects Around Supporting a Culture of Innovation
So you think you’re supporting a culture of innovation within your organization? Here are three disconnects to look out for.
February 22, 2023
|

Why Embedding Inclusive Design From Start to Finish Is Critical
The journey towards an inclusive design outcome must start by engaging those for whom the design is intended.
February 17, 2023
|

Investing in Lifelong Learning Experiences to Reenergize our Workplaces
As a process, lifelong learning hasn’t translated itself into our culture or manifested itself in our everyday lives.
February 17, 2023
|

How Office-to-Residential Conversions Could Revitalize Downtown San Francisco
One of the easiest ways to create diversity in office-centric downtowns is to convert existing office buildings to other uses. Residential is an obvious choice.
February 16, 2023
|

3 Surprises Impacting the Return to the Office
Our workplace research uncovered three surprising truths impacting the new role of the office, and what might bring workers back.
February 13, 2023
|

What Is WiredScore and What Does It Mean for Your Building?
In a highly competitive market, building owners should consider implementing a more robust digital infrastructure through the global standard for technology in buildings.
February 09, 2023
|

Building Buzz: Strategies for Energizing the Workplace
How do you design for “buzz” in the workplace — that intangible phenomenon that bridges the anticipation of coming into work with the experience once you’re there?
February 09, 2023
|

No Single Solution Will Save Cities. Three Just Might.
By focusing on the interconnected issues of reimagined workplaces, attainable housing, and safe and accessible transportation, we can help cities reach vibrant new heights.
February 08, 2023
|

From College Playoffs to the Super Bowl: How Can We Reimagine Live Sports Experiences?
As sports fans journey back to stadiums and arenas, what are their new expectations for game day experiences? Gensler’s Sports Experience Survey offers insights.
February 08, 2023
|

Bridging the Gap Between Theory and Practice: Lessons From U.K. Architectural Apprentices
For the U.K.’s National Apprenticeship Week 2023, we spoke with Gensler London’s graduated apprentices about their journeys.
February 08, 2023

Destination Aldgate: Reinventing London’s Central Business District
Here’s how we developed a strategic vision to address the rapid growth of commercial and residential development and bring out the Aldgate Connect BID’s distinct identity.
February 07, 2023
|

From Vacancy to Vibrancy: Reimagining the Future of Downtown San Francisco
We look at a new vision for downtown San Francisco: a central business district transformed into a vibrant, sustainable, and resilient mixed-use neighborhood.
February 06, 2023
|
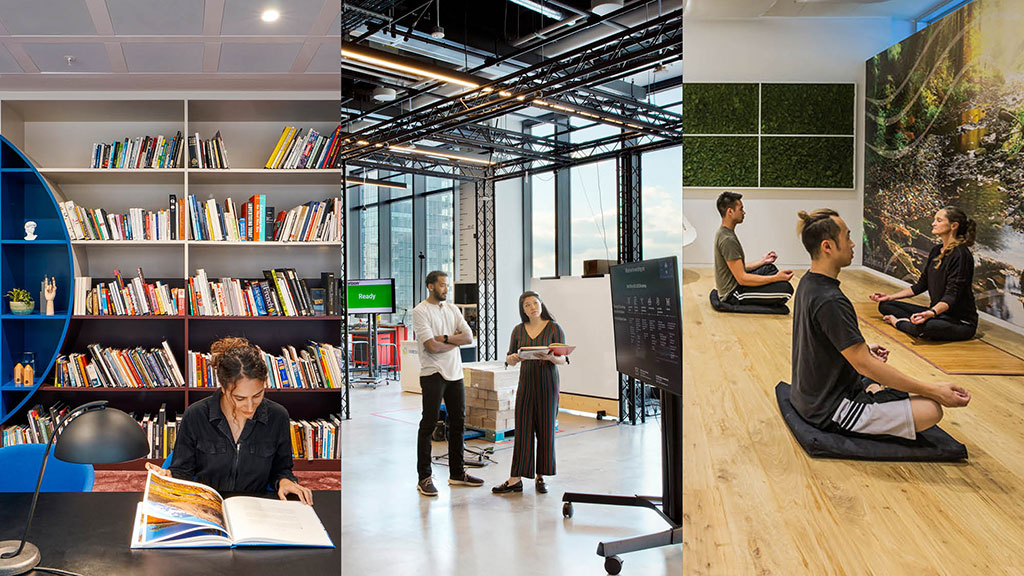
10 Spaces That Are No Longer Optional to Create a Great Workplace Experience
What amenities can bring people back to the office? Here are 10 spaces that have the greatest impact on workplace effectiveness and experience.
February 06, 2023
|

Creating Spaces That Evoke Joy Through Immersive Design
How can physical spaces evoke joy? Design needs to incorporate multiple characteristics and fully engage our senses to be considered an immersive experience.
February 03, 2023
|

Getting to the ‘S’ and the ‘G’ in ESG Through Design
Designing for the ‘S’ (Social) and fueling the impact of the corporate ‘G’ (Governance) in ESG can help realize positive, measurable outcomes in the community.
February 02, 2023
|

Unlocking Hidden Value: How Cities and Developers Are Partnering to Turn Vacant Offices into Residential
Vacant office spaces are a burden for cities and developers. Here’s how to convert vacant office buildings into new housing.
January 31, 2023
|

Debunking Three Myths About Designing for Older Adults
As part of a Gensler research initiative, we embarked on a study to learn more about the attitudes and living preferences of independent adults over age 55.
January 24, 2023
|

Nature + Nurture in the Inclusive Workplace
As tech companies plot their partial return to the workplace, some are ready to embrace our latest challenge: How we take insights from the past two years and use them to design joyful, inclusive work environments?
January 23, 2023
|

How Can Companies Leverage the Sublease Market to Gain Access to Prime Office Space in Downtown Toronto?
With companies reevaluating how to meaningfully reengage with the workplace, many enticing opportunities are appearing on the sublease market in the Greater Toronto Area.
January 23, 2023
|

As We Return to the Workplace, It’s Not the Same — What Works? What Doesn’t?
An effective, well-designed workplace can impact the overall work experience. Here's a look at what's working — and what's not — as we return to the office.
January 23, 2023
|

Using Algae to Offset the Carbon Cost of Data Centres
Data centres use about 1% of the planet’s electricity and are responsible for about 0.25% of the world’s carbon footprint. What if there were a way to capture those carbon emissions within the building itself?
January 20, 2023
|

8 Trends to Watch: Economic Headwinds Will Help Us Focus on What We Value
We need to let post-pandemic workplace patterns and attitudes evolve while planning for future flexibility, nuance, and performance.
January 20, 2023
|

Marriott International Provides a Model for the Workplace of the Future With Their Hospitality-Infused Global Headquarters
Marriott’s reimagined global headquarters fuses hospitality and workplace design to draw people back to the office with a work experience that captures the energy and ambiance of a vibrant hotel.
January 18, 2023
|

The Rise and Fall of the Corner Office: Does Status Still Matter in Workplace Design?
Since social status has been linked to employee engagement and job satisfaction, it may be an interesting tool to revisit to attract people back to the office.
January 13, 2023
|

Bob Weis, Former President of Walt Disney Imagineering, on Immersive Experiences and the Story of Our Cities and Spaces
Now at Gensler to lead Immersive Experience Design, Bob talks about how physical experiences are connecting people to place in inspiring new ways.
January 12, 2023
|

What Can Cities Do to Bring People Back to Public Transit?
While most city dwellers feel positively about their city’s public transit system, fewer feel that it provides a great experience.
January 11, 2023
|

How the Flight to Experience Can Unlock Value for Commercial Office Buildings
It’s time to rethink the traditional commercial office building model — by redefining “quality” in office buildings and creating workplaces that foster memorable experiences for today’s tenants.
January 11, 2023
|

Construction Costs Continued to Climb Through 2022
Construction costs have experienced many disruptive pressures due to the pandemic – from limited labor to stressed supply chains to stubborn inflation pressures. While the industry still finds itself challenged by these pressures heading into 2023, increasing interest rates and the corresponding downward pressure on demand may finally provide some relief.
January 09, 2023
|

Strategy: The Unseen Partner for Workplace Design
Clients are looking to support talent through new policies, work point design choices, service design strategies, amenities, and locations.
January 05, 2023
|

Trends to Watch: What’s Next for the Future of Workplace and Workplace Design
Clients are experimenting with hybrid work, policies changes, spatial needs, and how to create a workplace that supports what workers need. Here’s what’s next for the future of workplace and workplace design.
January 04, 2023

The Trends Defining What’s Next for Stranded Assets and Building Transformation
Owners and developers are considering how to convert Class B and C office buildings that sit vacant as tenants flock to modern, amenity-rich properties.
January 03, 2023

A Shifting Workplace Paradigm for the New Year
In this time of constant change and challenge, people want to spend their time in environments that maximize the way they live, work, play, and collaborate. Our latest research sheds light on an emerging trend in how people and companies are using their space.
January 03, 2023
|

Hot Topics From a Year of Transformation and New Ideas
Now more than ever, people are attuned to how physical space shapes experience. As we prepare for the new year, we’re looking back at ideas with the biggest impact in 2022.
December 22, 2022

Trends to Watch: Accessible and Inclusive Design Will Draw Workers Back to the Office
Here’s how workplace designers can play a vital role in creating inclusive spaces that are welcoming of all people and all abilities and supportive of employee well-being with the right mix of amenities and spaces.
December 21, 2022
|

Rethinking Las Vegas, Its Hidden Potential, and Future Promise: A Conversation with Brett Robillard
Brett Robillard, a principal and studio director at Gensler’s Las Vegas office, discusses Las Vegas’ ripe potential for growth and expansion, its many misconceptions, and what a new kind of design thinking can bring to the future development of the city.
December 20, 2022
|
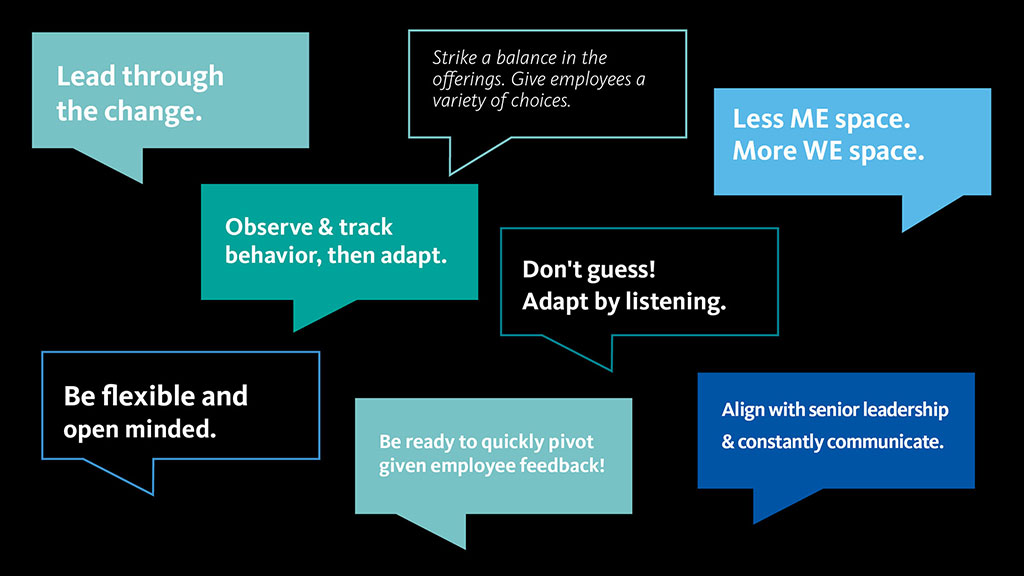
What’s Next for the Office? Here’s What Corporate Real Estate Executives Say.
Gensler’s survey of CoreNet Global end users aims to understand what CREs are currently implementing or considering across their office portfolio and how plans will impact their real estate footprint.
December 16, 2022
|

Thinking Outside the City: Why Transforming Stranded Assets Can Unlock Value in the Suburbs
With millennials and young families leaving cities for the suburbs, transforming stranded assets such as office parks and retail malls into mixed use districts is a major opportunity to add value.
December 16, 2022
|

What the Rise of Micromobility Means for the Future of Cities
One trend that emerged from Gensler’s survey of 15,000 residents in 30 cities may change how we navigate urban life: micromobility is more popular than ever before.
December 15, 2022
|
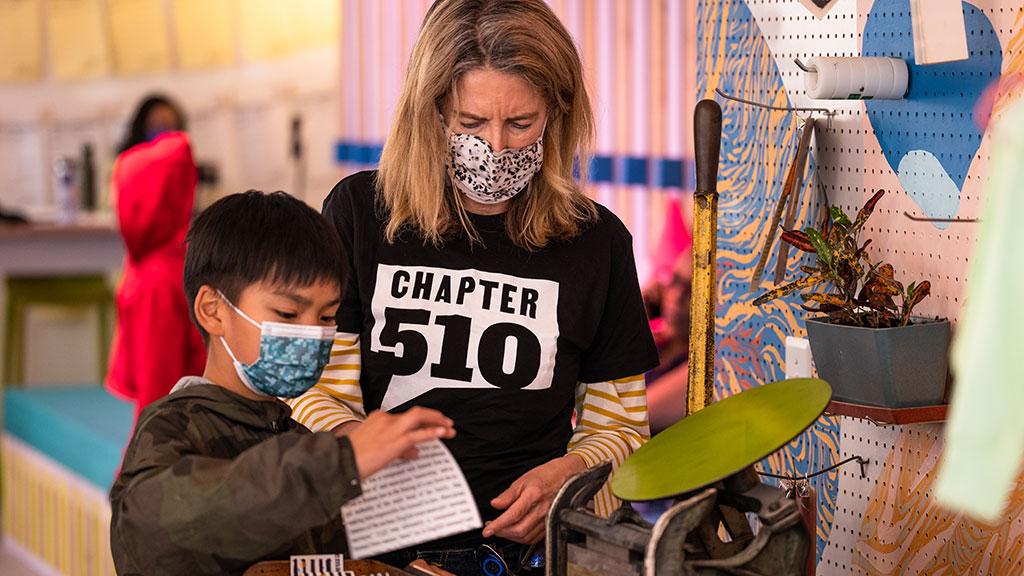
Designing for Social Impact in Our Communities
The Gensler Community Impact Awards celebrate the remarkable achievements of teams across the firm in pro bono, low bono, mentoring, and research projects that align with the Gensler Model of Community Impact.
December 14, 2022
|

A Holistic Approach to Community Impact in Washington, D.C.
Our Gensler DC Community Impact group has developed a key partnership with Kelly Miller Middle School in Ward 7 to provide holistic support to the students and their families.
December 14, 2022
|

What Gensler’s Latest City Pulse Says About Sustainable Transportation
What can cities do to promote more sustainable transportation options? Gensler's City Pulse data reveals that it may come down to convenience and cost.
December 07, 2022
|

Experimentation in the Workplace: Adopting a Software Mindset
To deliver a work system that's designed for success in the current hybrid work environment, design teams must adopt a rapid cyclical development approach that builds a deep understanding of changing leadership aspirations, functional needs, and cultural workstyle norms.
December 07, 2022
|

What Gensler’s Recent U.S. Workplace Survey Reveals About What’s Working — and What’s Not — as Workers Return to the Office
Employees say they need to come into the office more often to maximize productivity. The right mix of experiences could accelerate their return.
December 06, 2022
|

To Further Your ESG and Carbon Commitments, Start With Signage
When looking for an impactful, actionable, and timely way to support ESG and carbon goals, we suggest starting with a fundamental, yet often overlooked tool: signage.
December 05, 2022
|

Activating a Former Gas Station as a Community-Forward Urban Retreat
When the Denver Beer Company approached us to design a new restaurant, ice creamery, and beer tasting room, the concept was to create an inclusive gathering space for all.
December 01, 2022
|

Financial Firms’ Shifting Priorities: Investing in People and Purpose Through ESG Commitments
Companies are implementing ESG frameworks to attract top talent and to protect bottom lines. Here’s how we are helping clients put those commitments front and center.
November 23, 2022
|

How Desire for Experience Is Driving the Flight to Quality
People want to be in spaces that maximize how they live, work, and socialize, which is driving demand for Class A buildings. We’re seeing a flight to quality — and experience.
November 22, 2022
|

High Street Place: From Unused Office Lobby to Vibrant Culinary Destination
In the heart of Boston’s Financial District, we partnered with the Rockpoint Group to transform an underutilized atrium between two Class A office towers into an 18,000-square-foot, Art Deco-inspired food hall.
November 21, 2022
|

Consumer Goods Companies Are Now Competing for Tech Talent
As more consumer goods companies look to diversify their talent pool, how do they compete with the new expectations and needs of workers? Here are three workplace strategies for creating an authentic sense of purpose and connection.
November 17, 2022
|

China’s Honor Life Store Shows How Retail Design Acts as a Cultural and Brand Lens
The new Honor Life Store in China is an immersive, experiential retail format that is an extension of the brand, designed to showcase the possibilities that Honor’s technology enables.
November 11, 2022
|

3 Strategies to Stem the Tide of Rising Global Temperatures
All segments of the built ecosystem must change direction to stem the tide of rising global temperatures — whether it’s how we build new cities, re-adapt existing cities, or protect cities in vulnerable regions.
November 09, 2022
|

Murals of Joy: How Custom Murals Can Improve Well-being in the Workplace and Beyond
Inspiring and integrating, murals are complex tools of design that can enliven an entire workplace and integrate a community with the environment that surrounds it.
November 07, 2022
|

Using Design to Improve the Transit Experience for Los Angeles Metro
Gensler teamed with LA Metro to create a series of innovative Integrated Station Design Solutions to improve the overall transit experience.
November 02, 2022
|

A Targeted Approach to Reimagining Central Business Districts
We don’t yet have all the answers for how to remake CBDs, but we our research and commercial real estate trends indicate that we need a shakeup.
October 24, 2022
|

The Urban Block Club: A New Model to Revive Our Central Business Districts
To revitalize cities, we can reimagine a resilient, community-focused approach that brings different property owners within a district or block to work with each other and the city to create viable developments.
October 21, 2022
|

The Infinite Office: How the Metaverse Connects Us, in Real Life
How might the metaverse allow us to make hybrid work better, provide new value in our retail relationships, and reconnect to our cities and each other? Our Digital Experience Design leaders explore possibilities.
October 20, 2022
|

The Hospitality-Driven Workplace
To better attract, engage, and retain talent in the workplace, it will be critical that organizations take a cue from hospitality, viewing employees as valued guests.
October 20, 2022
|

Exploring the Future of Workplace Metrics With Machine Learning
When guided by theory and research, emerging data platforms and data science tools, such as machine learning, can reveal new insights about how to design effective workplaces.
October 18, 2022
|

Behind the G: The Importance of Design Technology
A group of graduates in the London and Birmingham offices spoke with members of our European Design Technology (DT) team about their roles, specific expertise, misconceptions related to design technology, and where the future of DT might take us.
October 13, 2022
|

The Airport of Choice
For those who elect to travel, having the ability to curate a custom airport journey based on individual needs and preferences could encourage people to return to the skies.
October 12, 2022
|
Gensler Voices: Francisco Gonzalez on Why It’s Vital to Design Inclusive Spaces
Francisco Gonzalez, co-managing director, Gensler Washington, D.C., discusses his career path, and the impact design and architecture can have on our communities and the human experience.
October 12, 2022

The Nth Space: Hybrid Work and the Future of Gas Stations
As we’re seeing with many workers, remote work doesn’t only mean working from home — it means working from anywhere. That’s one reason gas stations, with their abundance and strategic distribution across the urban landscape, are primed to be reconfigured as third places — new fixtures of our cities that offer a flexible and sustainable solution to building tomorrow’s workplace ecosystem.
October 11, 2022
|

Gensler Voices: Ana Salazar on How Her Hispanic Heritage Ignited a Passion for Sustainability
Ana Salazar, design manager for Gensler Houston, chats about her upbringing in Monterrey, Mexico, her journey to Gensler, and how it all influences her current approach to design.
October 11, 2022

Dual-Brand Hotel PIPs Create Design, Financial Opportunities
Hotel developers are interested in dual-brand Property Improvement Plans, which can bring market-driven properties back to financial viability faster than ground-up hotels.
October 03, 2022
|

The Future of Office and Lab Space Has No Boundaries
As more life sciences companies aim for increased transparency for the sake of engagement, talent retention, and breakthrough innovation, the boundary between workplace and laboratory blurs.
September 26, 2022
|

Rethinking What Museums Can Do for Communities — and How We Design Them
With the right vision and design experience, museums can be spaces to both educate and entertain audiences in deeper ways, inspiring them to be stewards of our communities.
September 14, 2022
|

From Briefing to Experience, Designing Today’s Customer Experience Center
For many organizations, from technology, to finance, to sports teams, Customer Experience Centers (CECs) are the catalyst for developing and fostering customer relationships.
September 14, 2022
|

A Future Vision of Workplace Metrics
New sources of data and workplace analytic tools will help us assess a “people-centric” workplace, using organizational outcomes as workplace performance KPIs.
September 12, 2022
|

The Carbon Innovations Hiding in Plain Sight
Gensler Global Co-Chair Diane Hoskins addresses the carbon footprint of concrete and explains how we’re pushing the concrete industry to reduce carbon emissions.
September 09, 2022
|

Product Design Gets Redefined
When Creating a Wall for All
Working with our client, we designed a demountable partition system that allows employees to easily restructure and repurpose the many open areas of an office.
September 01, 2022
|

How the Bipartisan Infrastructure Law’s FAA Airport Terminals Program Will Impact U.S. Airports
Here’s how the first $1 billion in funds from the Bipartisan Infrastructure Law's FAA Airport Terminals Program is being used to improve the traveler experience — and how other airports can take advantage of these new opportunities.
August 30, 2022
|

How Local Governments Are Transforming Green Building Policies — and How to Prepare
Here is a primer on where green building policies came from, what they mean, and where they’re likely to go in the future.
August 18, 2022
|

Embracing Senior Living in the Urban Mix
In the next 20 years, the over-65 population will double — as seniors make up more of our urban communities, we need to reconsider the role that active aging and senior living developments can play.
August 17, 2022
|

Together, EVs, AVs, and Multimodal Transportation Will Create More Vibrant Cities
We want the act of moving around our cities and communities to be convenient, quick, clean, accessible, and inclusive. So what does that look like, both today and in the years to come?
August 15, 2022
|

The Future of Work Is Seasonal
Our lives are influenced by seasonal and cyclical events, so what if our work behaviors followed suit? We explore the possibilities of seasonal work.
August 09, 2022
|

What Workplace Can Learn From Airports
The best airports put a hyper focus on the passenger experience, so what if we leveraged the same lessons from the best in aviation design to create a more seamless, equitable workplace experience?
August 08, 2022
|

Are People the New Workplace Amenity?
Being with people may be the new workplace amenity — and a compelling reason to draw people back to the office for those that haven’t returned.
August 08, 2022
|

There’s No Place Like the Office: Infusing Hospitality Design Into the Workplace
In this episode of the Gensler Design Exchange podcast, we discuss the importance of infusing hospitality design into workplaces to turn offices into a destination, rather than an obligation.
August 05, 2022

What Sports Venues Must Do to Be Tomorrow’s Cultural and Economic Anchors
We will soon see sports and entertainment venues designed to be seamlessly integrated into districts. For both renovations and new venues, outward-facing activation will be key.
August 03, 2022
|

The Housing Crisis: Finding Hope in Innovation
The pandemic exacerbating the housing crisis in many U.S. cities. For residential architects and designers to make a difference, we must embrace solutions like modular construction, adaptive reuse, and progressive legislation.
August 03, 2022
|

How Affinity Districts Find Purpose in a Transactional World
Affinity districts offer an alternative to the purely transactional approach of selecting a place to live or work and herald a return to values-based urban design.
August 02, 2022
|

How LinkedIn’s Omaha Headquarters Fosters Community and Equity
Designing a thoughtful brand experience is a powerful tool in building engagement and alignment between employee and purpose.
August 01, 2022
|
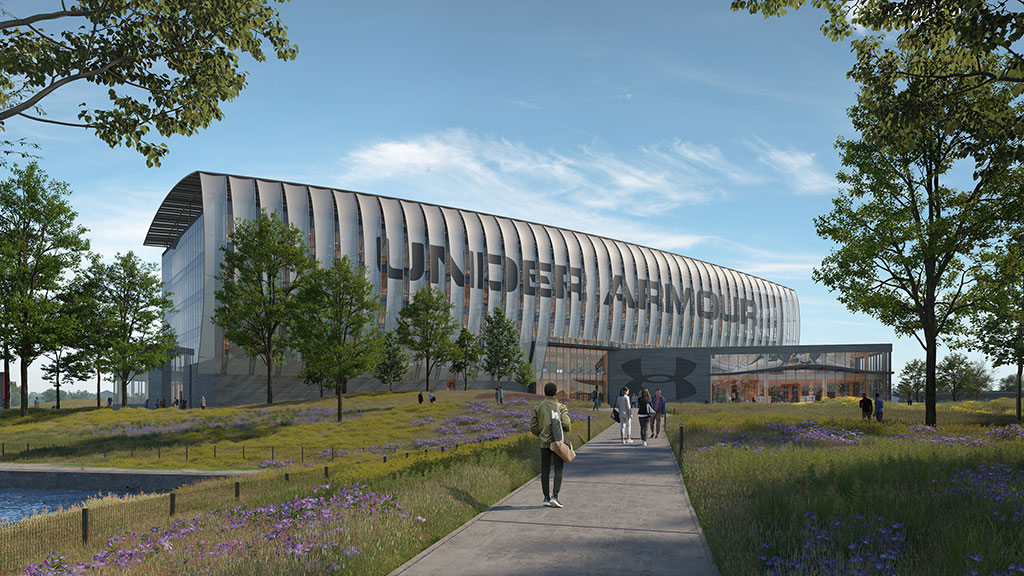
Is Mass Timber the American South’s Best Kept Secret? Not for Long.
The southeast United States is emerging as a serious contender in the mass timber market, where several large-scale campus projects are poised to redefine sustainable architecture.
July 29, 2022
|

Shopping Malls Are Dying — Here's How to Bring Them Back to Life
Malls are not necessarily dead; what’s changing is the expectation of what they should or could be.
July 27, 2022
|

How Brands Can Amplify a Purpose-Driven Culture
Purpose is a key factor in building a strong culture, driving success, and engaging employees. Here are three ways brands can create a purpose-driven culture.
July 27, 2022
|

Hybrid Retail: 6 Principles for Meaningful Customer Engagement
Physical retail is essential to building meaningful connections with customers, but a mindset shift is necessary. Here are six principles for retailers to better engage in an increasingly hybrid world.
July 26, 2022
|

The Path Ahead: Leveraging Lessons for the Future of PreK-12 Learning
After more than two very challenging years for education, the question in front of us now is: what lessons have been learned about our children’s education and the role of schools in our communities?
July 21, 2022
|

Product Design Gets Graphic:
A Story of Life Safety
Many clients want custom glass graphics, but costs can be significant, and the process can take months. We partnered with a trusted manufacturer on a prepackaged program to offer a practical and convenient solution.
July 21, 2022
|

How Inside-Out Design Can Boost the Cultural Experience
Designing spaces that are meant for the public requires a different approach — one that is bespoke, transparent, and equitable.
July 14, 2022
|

What Senior Living Has to Say about Health and Well-Being in Design
Senior living design prioritizes health and well-being and forces us to think deeply about the experience of the end user without taking their abilities for granted.
July 13, 2022
|

4 Strategies for Amplifying Health and Well-being in Residence Halls
Gensler’s design for an on-campus housing project for CSULB takes a holistic approach to sustainability, focusing on student health, well-being, and equity.
July 13, 2022
|

Redefining Learning for the 21st Century
Right now, we have the perfect opportunity to reassess the learning process and take a broader view of what it means to be a learner in the post-pandemic age.
July 12, 2022
|

Why It’s Time to Demand More From Our Workplace Experience
Here are 10 considerations for reimagining the workplace to deliver more from technology, be bold on resilience, and enhance our humanity, health, and communities.
July 11, 2022
|

Driving Inclusivity in Digital Content
We engaged diverse content creators to explore the topic of inclusivity and help shape perspective on how we can evolve both the way we work, and the work itself.
July 07, 2022
|

A YMCA Facility Reconceptualized to Prioritize Wellness and Community
As a facility that had to be reconceptualized and designed during the pandemic, the Holcomb Family YMCA in Spring, Texas is designed to help members maintain healthy lifestyles and stay connected with the community.
July 07, 2022
|
Behind the G: Approaches to Leadership
Behind the G is an opportunity for graduates in the London and Birmingham offices to meet and learn about the people at Gensler, the practice, and its culture
June 27, 2022
|

3 Steps for Setting the Stage for a Successful Hybrid Meeting
With hybrid work now a fixture of our professional lives, here are some best practices for creating a more seamless, effective hybrid meeting experience.
June 23, 2022
|

Houston’s First Innovation District Is Established With an Adaptive Reuse Approach
Reimagined to include Class A office space, shared workspace, classrooms, a lab, and maker space, the Ion launches a new, community-centered nucleus of innovation.
June 22, 2022
|

3 Considerations for Rethinking NYC Office Buildings
With outdated properties seeing higher vacancy rates and less interest in leasing activity, here are three considerations to rethink the potential of New York City office buildings.
June 21, 2022
|

5 Ways ESG Can Influence Design and Create Opportunities
Here’s how we’re expanding our understanding of ESG metrics so we can tangibly quantify the positive impacts design innovations can bring.
June 15, 2022
|

Revitalizing Stranded Assets to Build Vibrant Suburban Districts
With recent shifts toward suburban areas, civic leaders and real estate developers have an opportunity to create synergistic communities beyond urban downtowns that offer places to live, work, and play.
June 14, 2022
|

Climate Disclosure Mandates Will Irreversibly Transform Real Estate — and Supercharge the Low-Carbon Market
It has become clear that investors, driven by tenant demand and regulations, will be the force pushing the decarbonization of commercial real estate.
June 13, 2022
|

A Framework for Fostering Climate Resilience and Preparedness in the Built Environment
Within Gensler's U.S. Climate Action Survey 2022, we introduce a new roadmap for climate action through design that is anchored by four pillars: environment, economy, experience, and equity.
June 10, 2022
|

What Gensler’s 2022 City Pulse Survey Says About Hybrid Work and Urban Life
Findings from Gensler’s Spring 2022 City Pulse Survey show that people with remote work arrangements still tend to prefer city living — and that supporting flexible and hybrid work strategies at the city level is an opportunity to catalyze the rebirth of our downtowns and neighborhoods.
June 09, 2022
|

Labs and Sciences: Consider This for Adaptive Reuse
The lab and life sciences industry is seeing a spike in interest from real estate investors, but this specialized industry brings its own unique real estate considerations.
June 08, 2022

5 Strategies for Converting Retail and Office Space into Ambulatory Surgery Centers
Here are five strategies to convert vacant or underutilized retail and office properties into outpatient care facilities that support a positive and efficient experience for both patients and staff.
June 07, 2022
|

Product Design Takes
a Bathroom Break
Hygiene enhancement is a cardinal objective when designing most products intended for public restrooms, but it’s not the only way to bolster end user confidence and comfort.
June 06, 2022
|

The Impacts of Affordability, Remote Work, and Personal Safety on Urban Life
How are factors like affordability, remote work opportunities, and personal safety affecting people’s attitudes towards urban life? Gensler’s Spring 2022 City Pulse Survey examines how cities can meet the needs of all residents, now and in the future.
June 01, 2022
|

Living (and Thriving) at the Edge of Technology
Edge computing can improve performance, reduce costs, and help fuel the growth of next-generation technologies and applications.
May 27, 2022
|

How Willis Tower’s Repositioning Is Unlocking New Value and Reenergizing Chicago
Gensler’s Todd Heiser and Michael Townsend discuss “creating a building that is not about work, but about life” at Willis Tower — a 2022 Winner of AIA Chicago’s prestigious Design Excellence Awards.
May 26, 2022

How an Iconic Houston Park Helped Spark the Development of Downtown
The creation of parks and access to the outdoors has singlehandedly changed the way downtown Houston is accessed and utilized.
May 26, 2022
|

Mixed Use, Public Space, and the Future of Central Business Districts
With an influx of people to the suburbs and hybrid work here to stay, how do Central Business Districts reinvent themselves? Our research sheds light on the key characteristics residents want from cities and CBDs.
May 23, 2022
|

How to Make Your Office an Experience Multiplier
The new office must be an experience multiplier, a destination rather than an obligation. But how do you create that kind of place? Here are six strategies to make it happen.
May 17, 2022
|

How the Intersection of Architecture and Mobility Will Shape the Cities of Tomorrow
Recognizing a shared interest in solving complex urban mobility challenges, BMW Designworks and Gensler came together to explore a new range of design ideas for urban living in a project called Architecture X Mobility.
May 16, 2022
|

If Rush Hour Goes Away, How Should Public Transit Adapt?
A successful future for public transportation is likely to consist of highly fluid service that supports more trips throughout the typical day than just the daily commute.
May 12, 2022
|

Building a Better Academic Workplace
The 1,000-year-old academic workplace might finally have reached its breaking point — here’s how to reengineer it in a smarter way.
May 10, 2022
|

The Evolution of an Icon: Creating a New Experience at theMART
An inside look at theMART’s evolution as it takes on a new relevance to best serve the design and business communities of Chicago and beyond.
May 05, 2022
|

Hybrid Is Here to Stay: 5 Considerations for Creating a Better Hybrid Experience
Here are five reasons why hybrid work is here to stay, including design implications for creating compelling, people-centric hybrid experiences.
May 02, 2022
|
How Emerging New Workplace Realities Will Drive Corporate Real Estate Strategies
Coupled with Gensler’s workplace research, our survey of CRE executives offers valuable insights on return to office timing, the long-term impact on corporate real estate footprints, employer policies, and more.
April 29, 2022
|

3 Key Strategies to Build Your Brand and Culture in a Reimagined Future
Here are three key drivers of change and areas of focus for brands to reset and realign with people’s needs in a changing world.
April 29, 2022
|

Preparing for a Resilient Future Through Climate Action
Gensler’s Co-CEOs discuss how research-based design strategies can help cities and communities adapt to the changing climate.
April 27, 2022
|
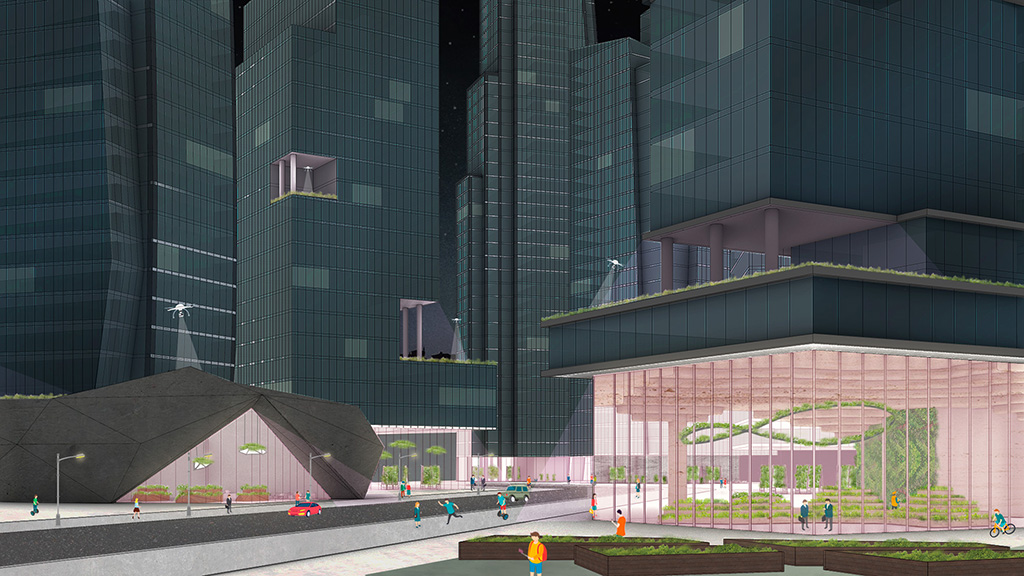
Cultivating a Food Resilient Future
Our research on food resilience started out with the focus on rethinking urban agriculture, identifying 12 opportunity areas where urban farms can be integrated into our cities.
April 27, 2022
|

The Case for Mass Timber: How First United Bank Is Creating a More Sustainable Future
Gensler’s design for several First United Bank projects in Texas and Oklahoma highlight the potential of mass timber as a sustainable, low-carbon material.
April 26, 2022
|

Designing an Innovation District for the City of Austin
Austin’s Innovation District unites education, entertainment, leisure, and sports. This type of urban, mixed-use center brings in new business and diverse populations, while enhancing the culture of a city.
April 25, 2022
|

Why Designing for Climate Action and Sustainability Is an Imperative
We sat down with the global leaders of Gensler’s Climate Action & Sustainability practice to discuss what’s next for climate action and sustainable design.
April 19, 2022
|

Inclusive Product Design:
Everyone Has a Seat at the Table
With careful planning and thoughtful design, the conference room experience will be seamless for all users, and everyone will get the most out of the space.
April 15, 2022
|

Built to Last: Improving Our Airports With the Bipartisan Infrastructure Law
With the Bipartisan Infrastructure Law criteria for next-gen air traffic control towers and terminals, we’re reminded that sustainable buildings should be built to last.
April 15, 2022
|

The Next Phase for Climate Action: An Embodied Carbon Revolution
We are working to influence the building industry by sparking demand for sustainable building materials to improve the resilience of global supply chains.
April 14, 2022
|

How the Building Industry Can Respond to the Terrible, No-Good, Very-Bad IPCC Report
The solutions we must embrace are not aimed at the 1% of iconic sustainable buildings, but rather they are intended to help us return to basic strategies across 99% of existing and future developments.
April 14, 2022
|

Gensler Voices: Joseph Joseph on Creating a Career in Digital Innovation
Joseph Joseph, Gensler’s global director of Design Technology, discusses how his identity and background have influenced his career path, and how diversity is built into the firm's culture.
April 11, 2022

Oakland’s Office Space Resurgence: Stitching the Old With the New for a Resilient Future
Oakland is continuing to transform its downtown urban core with a series of historic commercial building renovations that are driving a resurgence for creative office space and civic life.
April 08, 2022
|

5 Ways to Rethink the Future of Residential Development and Design
Gensler’s Residential Experience Index unpacks what makes a great living experience. Here are five key findings that demonstrate how we’re rethinking the future of residential development.
April 06, 2022
|

Net Zero Design Is the Key to Building a Resilient, Post-Pandemic Future
As we re-envision the way that buildings, developments, and even cities promote health, we must reimagine how the built environment supports the long-term resilience of our communities, livelihoods, and resources.
April 04, 2022
|

How Inclusive Design Supports Resilience and Climate Preparedness
We have an opportunity to design places that are inclusive, promote resilience, and make preparedness more accessible in the face of climate change events.
April 01, 2022
|

Visualizing Workplace Social Networks in Order to Drive Better Real Estate Decisions
Organizational network analysis (ONA) is an objective tool that can be used to understand how ideas and information flow among people in an organization. Here’s how we’re visualizing communication patterns to help drive better decisions about workplace real estate.
March 30, 2022
|

Understanding Supply Chain Challenges and Opportunities in Design and Construction
In this episode of the Gensler Design Exchange podcast, project management and technical experts offer insights and suggestions for making the design and construction process as smooth as possible.
March 22, 2022

The Future of the 20-Minute City
The “20-minute city” fosters connectivity to everyday resources by design. By designing through an ESG lens, we can create healthy, walkable communities for everyone.
March 21, 2022
|

Product Design With the World in Mind: Just What the Doctor Ordered
As one of the largest specifiers of furniture, fixtures, and equipment (FF&E), many of our product design clients are asking for our reporting requirements for embodied carbon in order to be more responsive to project needs.
March 18, 2022
|

To Reinvigorate Downtown Cores, Developers Should Adopt a Mixed-Use Mindset
To retain and attract post-pandemic tenants in urban cores, developers will need to adopt a mixed-use mindset, with a focus on the human experience first.
March 17, 2022
|

What the Workplace Sector Can Learn From Retail’s 20+ Years of Designing Hybrid Experiences
In an increasingly hybrid world, offices, retail stores, and other physical places need to bring people together and create community. Here are four lessons that the office sector can leverage from retail.
March 15, 2022
|

How TK Elevator’s New Workplace Spurs Connectivity Through Experiential Design
TK Elevator’s North America Regional Business Support Center merges experiential design with interactive spaces to achieve brand awareness and amplify community connection.
March 15, 2022
|

Modular by Design: The Promise of Prefab for Expressive Design
Designers are pushing the perceived limits of modular construction to build efficiently and safely while preserving time, cost, and materials. Explore prefab modular design for residential high-rises in Los Angeles.
March 11, 2022
|

3 Guidelines for Making Hybrid Meetings Work for You
For hybrid meetings to work, meeting formats shouldn’t just be an afterthought; to achieve an effective hybrid engagement for everyone, we need the right setup, the right facilitation, and the right purpose.
March 10, 2022
|

Understanding Changes in Project Costs Is Crucial to Designing Great Workplaces
For workplace developers, designers, and tenants who are rethinking the office in response to new ways of working, today’s cost challenges are particularly acute. Gensler’s 2022 U.S. Workplace Interiors Insights Report offers a deep look into today’s dynamic cost conditions, providing a path toward meaningful and actionable measures.
March 09, 2022
|

Design Strategies for Transitioning Back to Reopening
Across many parts of the globe, we are seeing mask and vaccine mandates being lifted. All this signals positive news for individuals and companies looking to get back to something resembling life in 2019.
March 08, 2022
|

Adaptive Reuse Brings New Vibrancy to Silicon Valley’s State Street Market
Adaptive reuse was a critical sustainable design strategy in designing the new State Street Market in Los Altos, California, transforming a dormant building into a vibrant community hub.
March 07, 2022
|

Reimagining Mass Housing Developments in Sub-Saharan Africa Through a Circular Cities Lens
For future African cities to be global magnets and domestic havens, it will be necessary to approach mass housing with a more resilient, regenerative, and circular mindset.
March 01, 2022
|

Leveraging Corporate Partnerships to Color Our Communities
In this episode of the Gensler Design Exchange podcast, we explore the power of corporate partnerships and youth development programming in strengthening support for our communities.
February 28, 2022

Multiuse, Connected, and Resilient Buildings Will Win Tomorrow’s Tenants
In this episode of the Gensler Design Exchange, design and development experts discuss how buildings can stand out and be more resilient in today’s competitive market.
February 25, 2022
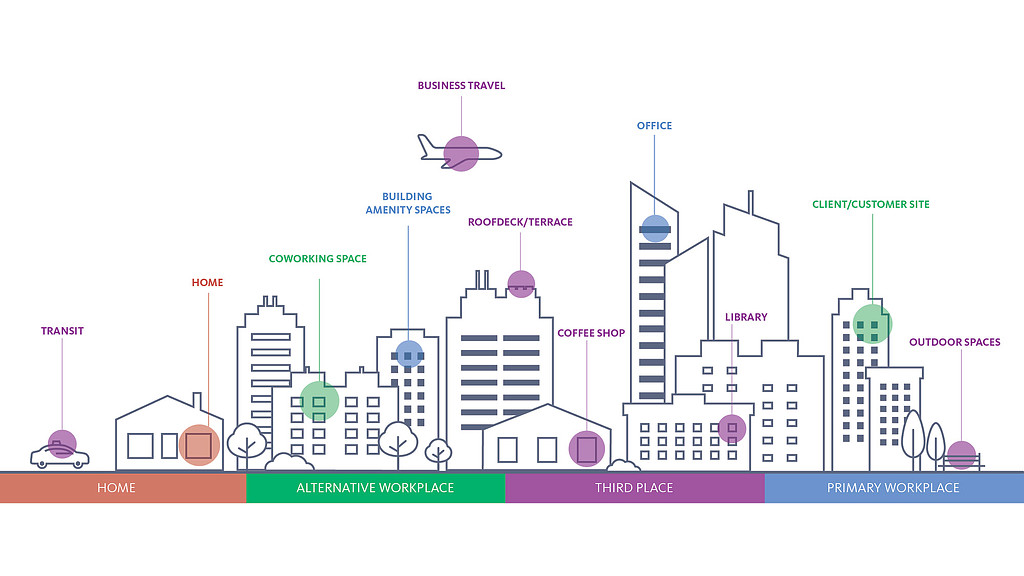
Why the New Workplace Ecosystem Is Key to the Future of Work
As we think about the future of work, consider a new workplace ecosystem — a Swiss Army knife approach to choosing the whole suite of places and spaces that provide the best environment for the work at hand.
February 24, 2022
|

New Gensler Workplace Survey Findings: Employee Expectations for Future Office Design and Culture
In this episode of the Gensler Design Exchange podcast, Gensler workplace experts share key findings from Gensler’s latest U.S. Workplace Survey and offer insights for a more meaningful future of work.
February 23, 2022

3 Lessons From Today’s Students That Will Shape the Future Workplace
Coupling findings from Gensler’s Workplace Survey and Education Engagement Index research, we’ve identified three key findings that the future workplace cannot ignore.
February 22, 2022
|
Gensler Voices: Eric Knowles on How Design Can Create a More Sustainable, Just, and Equitable World
We sat down with Eric Knowles, technical designer, Gensler Charlotte, to ask him about his career path and the impact that design and architecture can have on our communities and the human experience.
February 18, 2022

Gensler Voices: Heidi Davis on Why Diverse Teams Can Create New Narratives
We asked Heidi Davis, HR Director, Gensler’s North Central Region, to reflect on her career journey and the impact that design and architecture can have on our communities and the human experience.
February 16, 2022

A Workplace Designed for Trust and Empowerment
As the first new workplace designed to fully align with LinkedIn’s future vision, the company's Omaha, Nebraska offices point the way to what a fully dynamic, hybrid work environment looks like.
February 15, 2022
|

Innovation Districts, Affinity Districts, and the City of the Future
Here's how innovation is happening at a variety of scales, from affinity districts, to innovation districts, across cities.
February 14, 2022
|

The Future of the Museum Experience: Diverse, Inclusive, and Digital
In this episode of the Gensler Design Exchange podcast, we explore how museums are adapting to changing visitor expectations in an increasingly digital world.
February 09, 2022
|

Using Design Technology to Evolve Outpatient Healthcare Delivery
As providers assess the future of outpatient facilities, they can enhance data-driven design journeys with gFloorz 2.0, a computational product by Gensler.
February 08, 2022
|

The Key Elements of Successful Innovation Districts
What are the core fundamentals of innovation districts, and what makes them successful? People, place, and partnerships are key.
February 07, 2022
|

A Resilient Office Is an Occupied Office
In order to thrive, our downtown cores and buildings need to become more resilient, adaptable, and multiuse — considering efficient use of space and time as valuable factors in the resilience equation.
February 03, 2022
|

The Future of ESG in Architecture
A team at Gensler is changing the challenge of measuring the impact of ESG goals by developing design guidance and strategy to add clarity and specificity to ESG metrics.
February 02, 2022
|

Unlocking Workplace Purpose Starts With Self-Awareness
Companies that are making the most successful decisions about their workplaces are not following a prescriptive method or imitating others. They are doing what is right for them, responding to the specific needs of their business and employees.
February 01, 2022
|

The Lab Building of the Future is NEXT
The traditional method of designing new science buildings needs to evolve from what the building looks like, to how it needs to be optimized for each tenant.
January 25, 2022
|

Designing an Equitable and Connected Airport Experience for Every Traveler
In this episode of the Gensler Design Exchange podcast, four Gensler aviation industry experts explore how the pandemic has introduced airport design innovations in health, wellness, technology, and equity.
January 24, 2022

Learning From Home: 3 Key Lessons for the Future of PreK-12 Learning
How can the experience of working, parenting, teaching, and learning from home inform opportunities for future learning environments? Here are three key insights.
January 18, 2022
|

Product Design ‘Cleans Up’ and Office Hygiene Gets a Boost
As COVID-related office hygiene and cleaning protocols play a role in the return to the office, Gensler’s Product Development practice has a range of initiatives to help organizations take office hygiene to the next level.
January 10, 2022
|

How Are Companies and Employees Planning for the Future of the Office?
Amid a constantly evolving pandemic, how are companies and employees planning for a return to the office? Gensler's workplace survey research offers some insights.
January 06, 2022
|

Recruiting Robotics Against Climate Change
As part of the Department of Energy’s E-ROBOT initiative, we teamed up with a group of roboticists and builders to develop a flexible new tool and data platform that can streamline and simplify adaptive reuse and retrofit projects.
January 05, 2022
|

Why Is the Outlook on Telehealth So Complicated?
Telehealth was at the forefront of healthcare consults during the pandemic, but we’re not hearing enough on lessons learned. We have crucial questions that need answering but the experiment is still unfolding.
December 22, 2021
|

Using Technology to Help Solve Persistent Accessibility Problems in Public Transit
For the millions of people with visual, cognitive, or mobility challenges, accessing stations via elevators or even physically boarding a train or bus are daily concerns.
December 21, 2021
|

Real Estate Repositioning Priorities for Relevance and Purpose in a Changing World
The principles of flexibility, adaptability, and well-being are becoming vital in the attraction of future tenants and their employees, who will demand more balanced ways of working and living. Here are our 10 core principles that drive our work on repositioning and reuse projects.
December 21, 2021
|

Trends Shaping the Future of Mixed Use and Retail Centers
Mixed use spaces are in demand because mixed use provides flexibility, diversity, and a range of experiences. So, what’s next for mixed-use developments?
December 20, 2021
|

The Trends Redefining Sports Venues in 2022 and Beyond
Every fan coming to the game expects a higher level of experience. So, how can sports venue design enhance the spectator experience?
December 20, 2021
|

3 Trends That Are Here to Stay in 2022
In January, Gensler will release Design Forecast 2022 — here is a preview of a few design trends we anticipate rising to the fore in 2022.
December 17, 2021
|

Year in Review: Top 5 Topics of 2021
Throughout the year, we explored the responsibility we have as an industry to ensure the future health and safety of our cities and communities through the power of design. Here are our five biggest trends and topics from a year of rebuilding and reconnection.
December 16, 2021

How D.C.’s Community of Hope Family Health and Birth Center Supports Black Women
Birth centers can level the playing field for low-income women and women of color. Community of Hope offers health services regardless of one’s ability to pay.
December 13, 2021
|

What Urban Residents Say About COVID Variants, Wellness, and Cities
As the pandemic continues to evolve, what does the future of cities look like? Our City Pulse Survey offers some insights.
December 10, 2021
|

How Hospitality Can Revamp Financial Services and Professional Services Firms
With hospitality-inspired workplace design, financial firms can create a purpose-driven space that empowers employees, nurtures client relationships, and provides a competitive edge for attracting talent.
December 07, 2021
|

A Living Lab: Our Experience Designing Gensler Miami’s New Hybrid Office
Gensler Miami’s new hybrid office eschews traditional workplace planning methods to create an office space crafted around purpose and engagement.
December 07, 2021
|

Distribution Center Design and Last-Mile Logistics
Here are five considerations for setting up a successful logistics center that will meet the challenges in last-mile delivery.
December 03, 2021
|

Why Inclusive Design Is a Critical Advantage in the War for Talent
For companies who are looking to compete in the war for talent by delivering a positive employee experience, inclusive design is a critical consideration.
December 02, 2021
|

Cities Are Rebounding, But Their Relationship With Residents Is Changing
For the first time since we began surveying global city residents in May 2020 — during the early stages of the COVID-19 pandemic — living satisfaction is finally on the rise.
December 01, 2021
|

Delivering the Future at Pittsburgh International Airport
COVID-19 exposed the need to think about air terminals differently. New expectations and needs for airports mean they will evolve into multifaceted centers of activity for passengers, aviation staff, and the community at large.
November 30, 2021
|

How the New SFO Terminal Reflects the Needs of Travelers Post-Pandemic
San Francisco International Airport (SFO) Terminal 1 was undergoing a transformation long before COVID-19, including enhancements designed to improve the passenger experience.
November 29, 2021
|

Why Digital Transformation Is Critical for Retailers to Remain Relevant
Here are three key adaptations for retailers to embrace digital transformation and understand customer experience expectations, in-store adaptations, and digital engagement.
November 23, 2021
|

Unlocking What’s Next for Consumer Experiences
What are the future opportunities that brands should consider when designing retail and consumer experiences? We asked our retail leaders to share insights.
November 23, 2021
|

How Social Interactions Will Drive Retail Forward
The new retail environment will require an integrated design approach that will spark the social interactions we seek. Here are three key space considerations to support this.
November 22, 2021
|

From Parklets to Placemaking: Reimagining the Future of San Antonio
Parklets and other temporary design explorations can lead to more permanent solutions for creative placemaking, as well as increased pedestrian engagement and well-being in urban landscapes.
November 12, 2021
|

5 Trends CRE Leaders Can Use to Reimagine a New Workplace Reality
Here are five trends commercial real estate leaders are evaluating to drive business performance, innovation, and employee engagement.
November 07, 2021
|

How Companies Are Using the Office to Transition to the New Reality
By giving employees the power to tailor their own experience, we can create an office that’s ready for multiple futures.
November 05, 2021
|

The Future of Work Is Flexible
What does the future of work look like? If the pandemic has taught us anything, it’s that the future is flexible, and we must stay nimble so we can adapt to constantly evolving community conditions.
November 04, 2021
|

Navigating the Circular Economy: How Reusing Materials Saves Costs and Lowers Embodied Carbon
Here’s how companies can proactively decrease the carbon associated with materials in a building’s lifecycle and reduce debris and waste going into landfills.
November 03, 2021
|

Fighting Climate Injustice: 10 Strategies for Action
Gensler and the American Institute of Architects are both committed to an ambitious agenda in the fight against climate change. Climate justice refines that approach to ensure that no one community is unfairly impacted by the burden of climate change.
November 03, 2021
|

The Case for Adaptive Reuse: How The Link Drives Sustainable Design Strategies in Downtown Denver
We transformed a 1960s-era telecom office tower into a creative, modern, mixed-use office building at a fraction of the embodied carbon cost compared to building new.
November 01, 2021
|

The Morphable Office: Envisioning the Future of the Office Through an ESG Lens
What does the future office building look like? Gensler’s “Morphable Office” concept draws people back to the office and also addresses equity and climate change.
October 29, 2021
|

Why Physical Brand Experiences Are More Effective
By manifesting a brand’s vision and values within the workplace, employees understand the company’s soul, connect with its purpose, and become its champions.
October 28, 2021
|

Now Is the Time to Reinvest in Local Materials
COVID-19 could force us to improve construction’s supply chain impact.
October 26, 2021
|

Campus Masterplan 2.0: Including an Integrated Wellness Strategy
By creating a network of engagements and reinforcements throughout a student’s daily journey, academic institutions can normalize wellness and shift it from a place to go, to a state of mind.
October 26, 2021
|

Designing Performance Centers to Promote Well-being for Athletes
The sports industry has shifted beyond pure training facilities to establish athletic performance centers for “total performance” with spaces that support conditioning, treatment, recovery, and rehabilitation.
October 21, 2021
|

How Younger Workers’ Preferences and Workstyles Will Define the Future Workplace
The preferences and workstyles of our younger workers will increasingly define the future of the workplace for everyone. How will this impact how we work? We uncovered some distinct generational differences for how generations prefer to work and how they value the office differently.
October 07, 2021
|

The Future of Residential Design Must Balance Affordability, Satisfaction, and Experience
Among the factors impacting people’s decisions about where to live, what matters most? Gensler’s Residential Experience Index seeks to understand residents’ perspectives and uncover the factors driving housing satisfaction.
October 06, 2021
|

Stranded Assets: Realizing the Potential of Old Malls and Abandoned Office Parks
How can designers transform these properties into destinations that have environmental, social, and economic benefits?
October 06, 2021
|

Charting a Better Course for Senior Living
We want seniors’ years to be imbued with activity, purpose, and interpersonal connection. Here are four principles to help us create that future.
October 05, 2021
|

Hospitality’s Growing Influence on Mid- to High-End Residential Design
Here are five hospitality-inspired approaches for residential developers and designers to remain competitive and offer consumers complementary services that enhance their living experience.
October 04, 2021
|

Gensler Voices: Deysy Cruz Escobar on Why Underrepresented Communities Should Have a Voice in Design
We sat down with Deysy Cruz Escobar, technical designer, Gensler Atlanta, to ask her about her career path and the impact that design and architecture can have on our communities and the human experience.
October 01, 2021

Gensler Voices: Alex Fernández on the Art of Drawing to Envision a Better Future
We sat down with Alex Fernandez, design director, Gensler Boston, to ask him about his career path and the impact that design and architecture can have on our communities and the human experience.
September 29, 2021
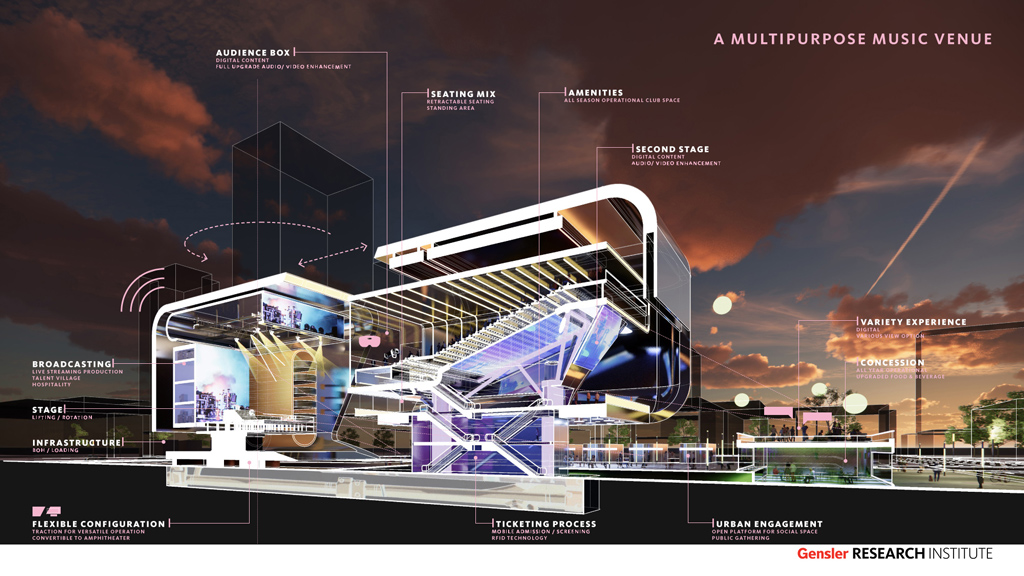
The Future of Live Music Venues
After analyzing pre-COVID trends, the industry’s pandemic response, and projections of post-vaccine preferences, we’ve identified six design and programmatic modifications that guide the development of the ideal music venue.
September 28, 2021
|

High-Tech, Low-Touch: Renavigating the Airport Customer Journey
Long airport lines aren’t just an inconvenience — they erode passenger confidence. Now, airports must reinvent themselves for a more seamless curb-to-gate journey.
September 28, 2021
|

Beyond the Lab Module: What Scientists Want From New-Age Lab Buildings
We interviewed four scientists with varied fields of research about their workplace experiences to learn how designers can create environments that meet their expectations and needs — as well as support their new ways of working.
September 27, 2021
|

Rethinking Longevity in an Age-Inclusive World
Design plays a key role in keeping older adults safe, connected, and engaged in their community. These strategies for reimagining longevity in an age-inclusive world cater to diverse needs and lifestyles of older adults.
September 23, 2021
|

3 Ways to Rethink the Outpatient Healthcare Experience
A variety of outpatient care options are fast becoming an integral part of today’s health system. We’ve delivered a study on outpatient care — here’s how we’re approaching things differently.
September 21, 2021
|

Gensler Voices: María José Tasada on How People and Culture Drive Design
We sat down with María José Tasada, project architect, Gensler Chicago, to ask her about her career path and the impact that design and architecture can have on our communities and the human experience.
September 20, 2021

Here’s Why Employees at Top-Performing Companies Need the Office
Top-performing companies support flexibility and encourage remote work, but they also value the role of the physical workplace to bring their talent together to achieve great results.
September 14, 2021
|

Designing a Workplace That Optimizes for Movement and Mobility
What would an office building that puts movement front and center be like? A new headquarters building designed for the American Physical Therapy Association explores that idea.
September 10, 2021
|

How to Create a Vibrant, Inclusive New City: The Story of Tysons, Virginia
Tysons, Virginia has a particular form of urbanism, one that simply isn’t replicated anywhere else. It has an uncommon diversity that goes beyond the surface level, and an inclusive architecture that sets a stage where life can be lived in a distinctly Tysons way.
September 08, 2021
|

Why Top-Performing Companies Are More Likely to Increase Their Real Estate Footprint Post-COVID
Even though delta changed the timeline, workers around the world still place a great deal of value in the physical workplace — and our newest data from the U.S. shows that people at the top performing companies in particular value the physical workplace and look forward to resuming in-person work.
September 07, 2021
|
_1629919083_1024x576.jpg)
How AT&T’s Discovery District Is Transforming Dallas’ Urban Core
By creating an immersive, mixed-use destination, the AT&T Discovery District reimagines the headquarters as a magnetic new public space, while breathing new life into Dallas’ downtown core.
August 31, 2021
|

Three International Lessons for U.S. Workplace Well-being
As organizations across the globe grapple with questions around the return to the workplace, figuring out how to adapt an organization’s culture is paramount.
August 27, 2021

New Design and Infrastructure Projects Are Unlocking the Northeast Rail Corridor
Investing in the Northeast Corridor — the most traveled rail corridor in North America — could unlock the East Coast’s full potential.
August 24, 2021
|

4 Ways Electric Mobility Will Reshape Our Cities
In the past few years, we've hit a tipping point for electric mobility. But the real game-changing story is largely being overlooked: electric vehicles have the potential to dramatically reshape our cities.
August 24, 2021
|

A Pandemic-Conscious Blueprint for Architecture
How uniform standards applied across the built environment can protect our communities from COVID-19 and future pandemics.
August 17, 2021
|

Lessons From India: 4 Interventions to Inform the Future Workplace
Gensler’s India Return to Work Survey 2021 reveals that workers in India are embracing a hybrid work model — but they face unique challenges and opportunities.
August 12, 2021
|

Meet the New 9-to-5: An Enhanced Approach to Hybrid Work
As we plot our returns to the workplace, there’s a need to craft new routines that address the new behaviors that we’ve honed in our remote work experiences.
August 11, 2021
|

Five Considerations for the New Lab of the Future
We have an opportunity to design a new kind of lab environment — one where ideation and innovation take center stage.
August 10, 2021
|

Why Circular Cities Play a Critical Role in Restoring Ecologies
To address pressing global challenges such as climate change, we must take a more regenerative, resilient approach to planning and developing our cities — one that is less linear, and more circular.
August 03, 2021
|

4 Emerging Patterns About Hybrid Work and the Future of the Office
As workers around the world continue to experiment with how and where they work in the face of ongoing uncertainty, Gensler's global Workplace Surveys uncover some universal truths and patterns about the hybrid future of work.
July 27, 2021
|

Gensler Voices: Maddy Crippen Shares an Athlete’s Perspective on the Olympic Venue Experience
We sat down with Maddy Crippen, Southeast regional marketing director, to ask about her experiences at the 2000 Summer Olympics in Sydney, and the Olympic venue experience from the athlete’s perspective.
July 26, 2021

Q2 Stadium Celebrates Austin’s Local Roots With a Unique Stadium Design
Austin’s Q2 Stadium is a 365-day destination and community asset that capitalizes on the city’s cultural heritage, natural landscape, and tech-forward growth.
July 20, 2021
|

Designing a Climate-Ready Headquarters for FIS in Jacksonville
Adaptable, resilient buildings will need to be able to specifically withstand sea level rise and storm surges long-term.
July 12, 2021
|

Gensler Voices: O'Lanre Smith Shares How World Travel Shaped His Architecture Career
We sat down with O'Lanre Smith, architect and technical director, Gensler Morristown, to ask him about the impact design and architecture can have on our communities, and his personal journey to becoming an architect.
July 09, 2021

Delivering Wellness on Campus so Students Can Thrive
Here are five considerations for colleges and universities to create a campus-wide wellness ecosystem that supports students where they are.
July 06, 2021
|

Gensler Voices: Asenath Yeung, Gensler San Jose
We sat down with Asenath Yeung, interior designer, Gensler San Jose, to ask her about her career path and how design can help raise awareness about subjects of wellness, equity, and inclusion.
July 02, 2021

Travel’s Resurgence: Here’s What Post-Vaccine Travel Will Look Like
What will post-vaccine travel look like in the U.S.? Gensler’s Hospitality Pulse Survey offers some insights.
June 29, 2021
|

Reimagining the Airport as the New Town Square
As passenger behaviors evolve and people seek to experience local culture, the airport will become a community hub where people can interact and gather, rather than a place solely for coming and going.
June 28, 2021
|
Gensler Voices: Brooks Morelock, Gensler New York
We sat down with Brooks Morelock, design director, Gensler New York, to ask him about his career path and how design can help raise awareness about subjects of wellness, equity, and inclusion.
June 25, 2021

Inside the World’s Largest Hospitality Company
Tim Grisius, Global M&A and Real Estate Officer at Marriott International, talks about Marriott’s evolution to become the world’s largest hospitality company; the hospitality industry’s path to recovery; Marriott’s new headquarters; and more.
June 24, 2021

Work From Home Needs a Home for Work
How can residential design evolve to support the growing at-home workforce? Gensler's Residential Experience Index offers some insights.
June 21, 2021
|

Why Now Is the Time to Rethink Workplace Amenities
As global enterprises prepare their return to the office, many are asking: what amenities might deliver the greatest returns in today’s evolving work landscape?
June 17, 2021
|
Bridging the Gap to Bring More Diverse Voices Into the Design Profession
Here are six lessons from our HBCU Student Design Charrette for bringing more diverse voices and talent into the design profession.
June 16, 2021
|

The Benefits of Converting Class C Office Into First Class Residential
In order to future-proof older buildings, clients need to make buildings more energy efficient, more resilient, and more vibrant to attract and retain tenants and talent.
June 14, 2021
|

Work From Home Product Design: How to Make a Desk Its Best
With more people working from home, the demands on the home office will evolve and consumers’ performance expectations for home office equipment — particularly the desk — are expected to increase.
June 11, 2021
|

The Fifth Façade: Rethinking Urban Rooftops for the Post-Pandemic Office Building
Rather than being a sign of exclusivity, rooftop spaces are becoming one of the biggest opportunities in real estate development and an essential part of any well-positioned office building.
June 11, 2021
|

Will Remote Work Trends Benefit Smaller, More Affordable Cities?
How can cities function as an attractive extension of the office in the age of “anywhere work?”
June 08, 2021
|

An 8-Step Model for ESG and Wellness in the Workplace
Helping people thrive at work through wellness design and initiatives may seem like an idealized goal. It’s not. It’s achievable and fundamental to ESG and wellness.
June 01, 2021
|

The Most Timeless Design Differentiator Is Technology
In the past year, we have seen our practice evolve and transform thanks to a number of proprietary computational design tools Gensler has developed.
May 25, 2021
|

Gensler Voices: Jon Park, Gensler Atlanta
We sat down with Jon Park, senior architectural designer, Gensler Atlanta, to ask him about his career path and the impact that design and architecture can have on our communities and the human experience.
May 21, 2021

Transforming Our Streets and the Public Realm Through Art and Programming
In 2020, we saw public space and art bring local and global communities together in new ways. How might we reimagine our streets and the public realm to steward more equitable and sustainable communities?
May 20, 2021

Lessons From China: What Hybrid Work Really Looks Like in Practice
The Chinese workplace is back open — and the experience of these workers holds lessons for the rest of the world as we consider what a hybrid workplace future really looks like.
May 19, 2021
|

Gensler Voices: Lily Diego, Gensler Detroit
We sat down with Lily Diego, design director, Gensler Detroit, to ask her about her career path and the impact that design and architecture can have on our communities and the human experience.
May 13, 2021

Designing a Mother’s Room Reentry Roadmap for All Scales of Workplace
Best practices to provide a purposeful wellness strategy for nursing mothers that destigmatizes and prioritizes a mother’s journey back to the office.
May 07, 2021
|

The New Hybrid Sciences Office Will Blend Tech Workplace, Hospitality, Brand Design, and Storytelling
To cultivate work environments that enable our sciences clients to innovate, we must look beyond traditional conventions of buildings and workspaces as places that optimize performance.
May 06, 2021
|

Gensler Voices: Lori Mukoyama, Gensler Chicago
We sat down with Lori Mukoyama, design director, Gensler Chicago, to ask her about her career path and the impact that design and architecture can have on our communities and the human experience.
May 06, 2021

5 Tips to Negotiate Your Next Commercial Lease Like a Pro
Here are five tips to bring better clarity and increase confidence when you approach your next lease transaction.
May 06, 2021
|

Gensler Voices: Fannie Cheung, Gensler San Francisco
We sat down with Fannie Cheung, technical director, Gensler San Francisco, to ask her about her career path and the impact that design and architecture can have on our communities and the human experience.
May 05, 2021
Building Brand Impression Through the Power of Memory and Multisensory Experiences
Here are three considerations for brands to tap into the power of memory to create multidimensional, multisensory experiences that leave a lasting impression.
May 05, 2021
|

Redefining Resilient Spaces Through Smart Material Selection
We discuss with Armstrong World Industries how we can decrease embodied carbon levels in the built environment simply by making smart choices about materials.
April 29, 2021
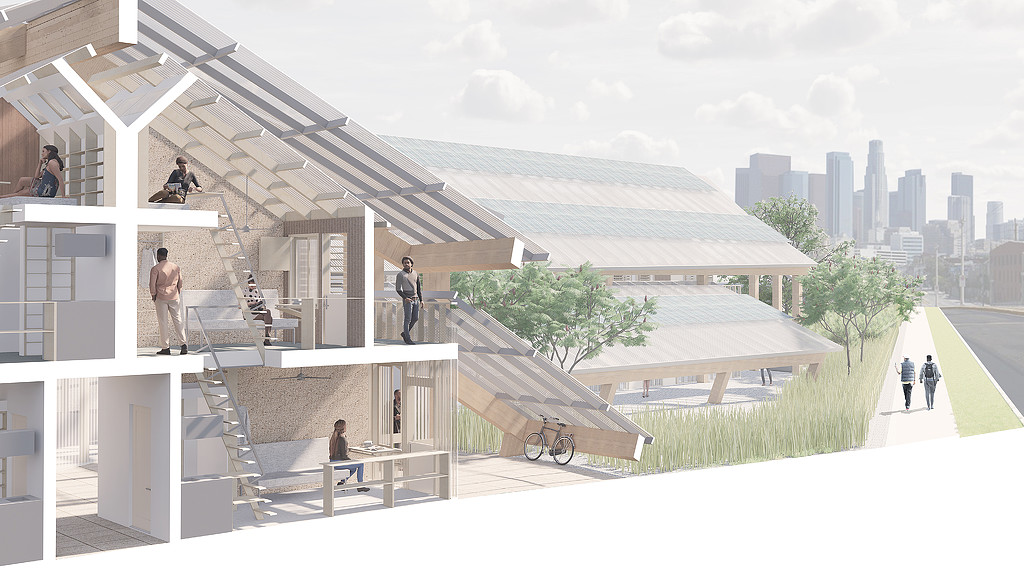
From Indifference to Serendipity: Experiments in the Art of Living Together
The pandemic presents an opportunity to rethink housing; architecture can and should play a critical role as an agent that tilts the outcome of each new project toward reconnection.
April 29, 2021
|

Gensler Voices: Willie Kirkpatrick, Gensler Houston
We sat down with Willie Kirkpatrick, architect, Gensler Houston, to ask him about her career path and the impact that design and architecture can have on our communities and the human experience.
April 26, 2021
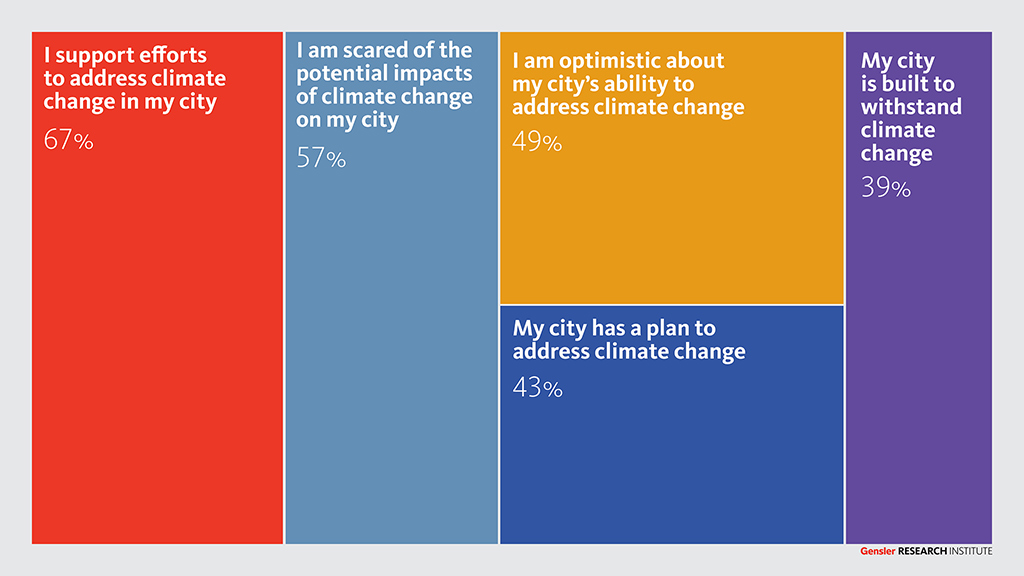
Urban Residents Around the World Support Efforts to Address Climate Change
Fewer than half of city dwellers feel optimistic about their city’s ability to combat the climate crisis — it's time for cities to meet the moment.
April 21, 2021
|

Reset: The Future Law Firm Workplace
The recent work-from-home experience has proven that attorneys can do without big private offices, lots of paper and files, and underutilized space. Now is the chance to reset the law office.
April 16, 2021
|
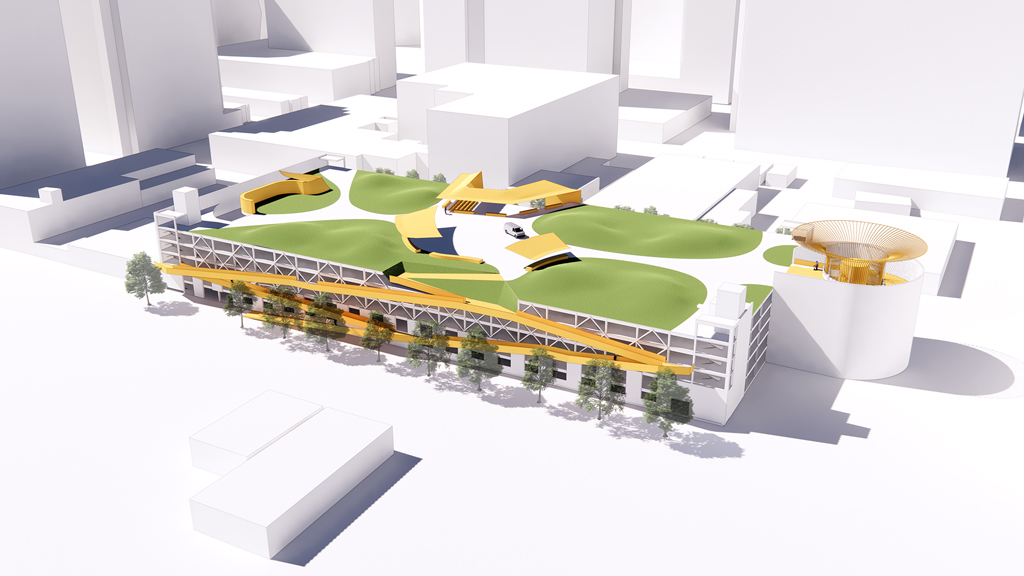
Converting a Parking Garage Roof Into a “People Deck” in San Jose
A proposal to convert a parking garage roof into a "people deck" in downtown San Jose offers a place where people can gather, exercise, and build community.
April 14, 2021
|

Closing the Digital Infrastructure Gap to Keep Cities Connected
Why has the gap between broadband infrastructure investment and access to connectivity persisted, and how can cities create information services pipelines to expand reach?
April 13, 2021
|

5 Principles for Retail Center Repositioning
Converting aging or underutilized retail malls into vibrant, mixed-use developments will unlock latent value and meet consumers’ changing demands.
April 13, 2021
|

Creating Resilient Urbanism With Streetscape Design
Our streetscape spaces have the potential to be vital agents in the fight against climate change and in creating livable cities.
April 09, 2021
|

Gensler Voices: Mustapha Williams, Gensler Chicago
Mustapha Williams, a technical designer at Gensler Chicago, shares what first sparked his design passion, how winning the Gensler Diversity Scholarship impacted his career, and why mentorship drives him.
April 08, 2021

How FOMO Is Driving People Back to the Office
With many colleagues getting back into the workplace, remote employees are experiencing a new kind of FOMO — the fear of missing out on useful updates, critical intel, and key connections.
April 02, 2021
|

Seizing the Opportunity to Rethink the Faculty Workplace
Faculty have been working, teaching, mentoring, and researching from home — or wherever they could find decent WiFi — for nearly a year. While most faculty agree that there are huge academic drawbacks to the current mode of teaching, there may be some important lessons that can guide us into the post-pandemic future.
March 29, 2021
|

Designing Schools for Equity and Engagement
To design the equitable and engaging post-pandemic school, we looked to three recent projects that exemplify the ideas of connectivity, adaptability, and choice.
March 26, 2021
|

Shaping an Equitable Future With USPS
How can the largest retailer in the country, the United States Postal Service, help create conditions to facilitate equity?
March 25, 2021
|

5 Considerations for Producing a More Equitable, Resilient Power Grid
When macro power grids fail, how can the equity of energy use be managed? Here are five considerations that can help evolve our power system to be more equitable and resilient.
March 23, 2021
|

Gensler Voices: Rhandi Green, Gensler New York
We sat down with Rhandi Green, job captain, Gensler New York, to ask her about her career path and the impact that design and architecture can have on our communities and the human experience.
March 22, 2021
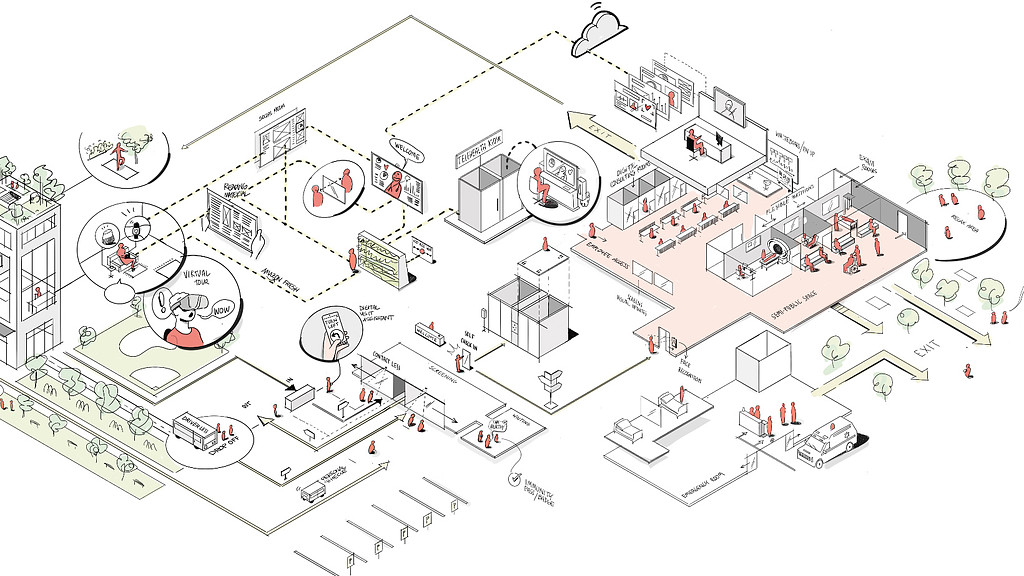
Digital Transformation of Healthcare Design
With healthcare technology woven into our daily lives, here are 4 fundamental principles for the next generation of integrated digital healthcare facilities.
March 17, 2021
|

Vuja De: Seeing the Office With Fresh Eyes
Because of the new perspective we've developed after working from home work over a year, we'll be seeing the office in a new light when we finally return.
March 10, 2021
|
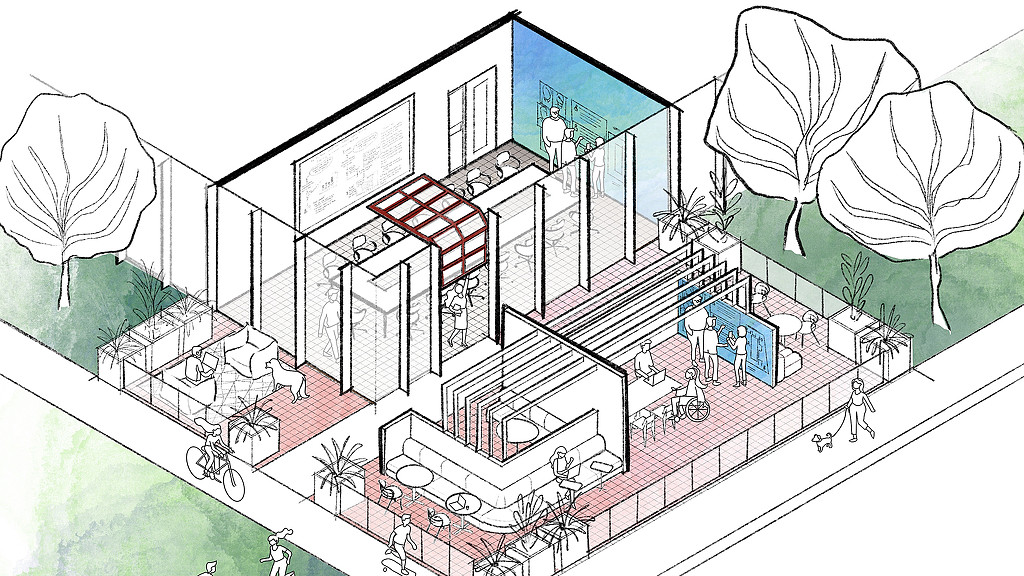
Sketching the New Hybrid Workplace
In this look at the future of hybrid work, Gensler architects and workplace designers shared their visions for the post-pandemic workplace and how it will function.
March 09, 2021

5 Design Interventions to Mitigate Virus Risk in the Workplace
To help return to work safely and reduce operational risk Gensler, collaborated with Haven Diagnostics to simulate how design impacts the spread of COVID-19 in the office.
March 08, 2021
|

Almaden Tower: Quickly Delivering an Innovative Office Building to Market
Innovative and tenant-responsive buildings can be quickly delivered without sacrificing design quality.
March 02, 2021
|

What We Can Learn From the Texas Weather Crisis About Design Resilience
What lessons can we glean from this crisis about designing more resilient structures, cities, and infrastructure in general?
February 26, 2021
|

Why Human Experience Is Critical to Las Vegas’ Reinvention
In a post-COVID age, how will a city that thrived on getting such a wide variety of people together now survive? Las Vegas has an opportunity to reinvent itself as a more diverse, inclusive, and engaging urban environment.
February 23, 2021
|

Why Ceilings Offer Clean-Air Solutions for a Post-COVID World
In this conversation with the CEO of Armstrong World Industries, we discuss how ceilings are an important part of the holistic approach to design we must take as we reimagine shared spaces in the future.
February 19, 2021

Egress Made Easier:
Product Design That Stands Out
By taking an approach that consciously stretches beyond the codes, Gensler is designing products that are more instinctive, more inclusive, and more hygienic.
February 12, 2021
|

The Mental and Physical Benefits of Our Plazas, Parks, and Sidewalks
Scientific studies back up what many already feel is true: our mental and physical health is inextricably linked to the connections between ourselves and the natural world, as well as social connections between individuals.
February 11, 2021
|

Why People-First Design Is Key to San Jose’s Future
In order to realize this future for San Jose and other cities, we need to act with design solutions that support our humanity.
February 05, 2021
|

Why Investing in Public Space Matters for Cities and Real Estate Developers
Right now, perhaps no other location or space type is in higher demand than pedestrian-friendly, outdoor public space.
February 02, 2021
|

Accelerating Momentum Around Climate Action With Every Person, Every Project, and Every Place
As designers and creators of the built environment, Gensler is committed to leading the charge in climate action and promoting a path towards net zero carbon.
February 02, 2021
|

The Power of the Pilot: A Low-Risk, High-Reward Real Estate Solution
The stakes are high for those making real estate portfolio decisions that will affect organizational culture and performance for years to come. But there’s a low-risk and high-reward solution: the pilot space.
January 21, 2021
|

Security and Democracy: Designing Public Buildings for Safety and Accessibility
Design has a key role to play in maintaining the balance between openness and security — in promoting both security and democratic values.
January 15, 2021
|

What’s Next for Higher Education? Esports and On-Campus Gaming Facilities
Prior to the pandemic, the world of esports was a nearly billion-dollar industry. For higher education institutions, it also created a new opportunity for recruitment by combining interest in competitive sports and gaming with real world training in STEM or related fields.
January 13, 2021
|

Real Estate’s Big Pivot to Science
For life science organizations in prime markets there’s a shortage of research-capable space. But owners and developers can make a pivot to science by repositioning buildings.
January 05, 2021
|

The Rise of Second-Tier Cities
Gensler's City Pulse Survey confirms that people are looking to leave global cities for more affordable, less dense cities that still offer culture and diversity, but at a smaller scale.
December 23, 2020
|

The Resurgence of Small- to Mid-Size Airports
Here are some strategies we’ve developed that cities and airports can use to revitalize their facilities in the post pandemic world.
December 15, 2020
|

Reduce, Reuse, Reclad at One Post Office Square
At One Post Office Square in Boston, an aging concrete office tower offered an opportunity to explore the value proposition in renovating aging buildings instead of building anew.
December 14, 2020
|

5 Insights on Creating Clear, Branded COVID-19 Signage
The current health crisis has added an influx of new signage to the ever-growing layer of promotional stimulation — and fatigue — many of us experience every day.
December 11, 2020
|

Real Estate Must Offer Human Experiences, as We Escape Virtual Lockdown Living
The recovery is an opportunity to realign real estate value with human experience.
December 10, 2020
|

Across the Globe, Workers Want a Hybrid Work Model
Gensler's Global Workplace Surveys uncovered some universal truths: most office workers want a hybrid work model, and the office is still the best place to connect.
December 09, 2020
|

Surprising Truths About the New Hybrid Workplace
Gensler's Workplace and Research leaders host a Q&A with Michael Gao, M.D. of Haven Diagnostics, on the return to the office and the future of the hybrid workplace.
December 08, 2020
|

Rebuilding Community in the Post-Pandemic World
When we can return to the office and resume other in-person activities, creating places for people to spend time together and rebuild community — not just in the workplace, but in every aspect of our daily lives — will be more important than ever.
December 08, 2020
|

Navigating a Fast-Changing Economy With a Workplace That Reinforces Purpose and Transparency
At City National Bank of Florida's Miami HQ, a workplace renovation uses the opportunity to build resilience, add transparency, and reinforce the bank’s purpose.
December 02, 2020
|

Reshaping the Retail Experience: Where Do We Go From Here?
Leading with service across all retail channels — whether physical, digital, or virtual — will result in deeper connections that drive loyalty and a better shopping experience
November 30, 2020
|

Record-Breaking Singles’ Day Sales Indicate a Solid Return to Retail in China
Brands all over the world can take a cue from the retail trends and opportunities emerging in China and the Asia Pacific region as they look ahead to what’s next.
November 30, 2020
|

New Types of Space on Campus
After spending more than eight months studying the shifting space needs at colleges and universities, we see several trends shaping the next generation of academic buildings.
November 25, 2020
|

Gensler Honored As First Firm to Win Three AIA COTE Top Ten Awards for Sustainable Design
Three Gensler projects were recognized for excellence in sustainable design at the 2020 American Institute of Architects Committee on the Environment (COTE) Top Ten Awards, including the Ford Foundation Center for Social Justice, UPCycle, and Etsy.
November 18, 2020

The Transformation of the Built Environment Requires a Digital Mindset
As our physical and digital behaviors continue to converge, design for the built environment will require not just advanced technology, but an entirely new digital mindset.
November 17, 2020
|
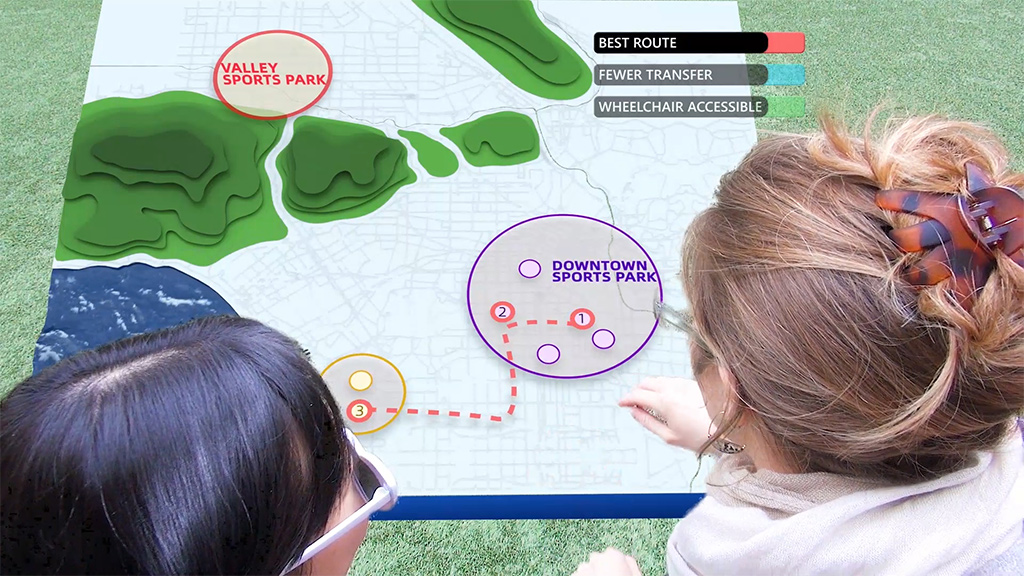
Mixed Reality Futures for Connected Transit
To stay relevant, transit systems must focus on new and novel ways to optimize rider experience.
November 17, 2020
|

Coworking Accelerates Life Science Startup Timelines
Scientific entrepreneurs face high rents, lab construction, and equipment costs, plus the operational and safety concerns of starting a research lab. Here’s how to think about developing laboratory coworking.
November 09, 2020
|

With Face-to-Face Meetings Sidelined, What’s Next for Experience Centers?
We are asking critical questions to understand how experience centers can thrive during this time of limited travel and infrequent face-to-face interactions.
November 06, 2020
|
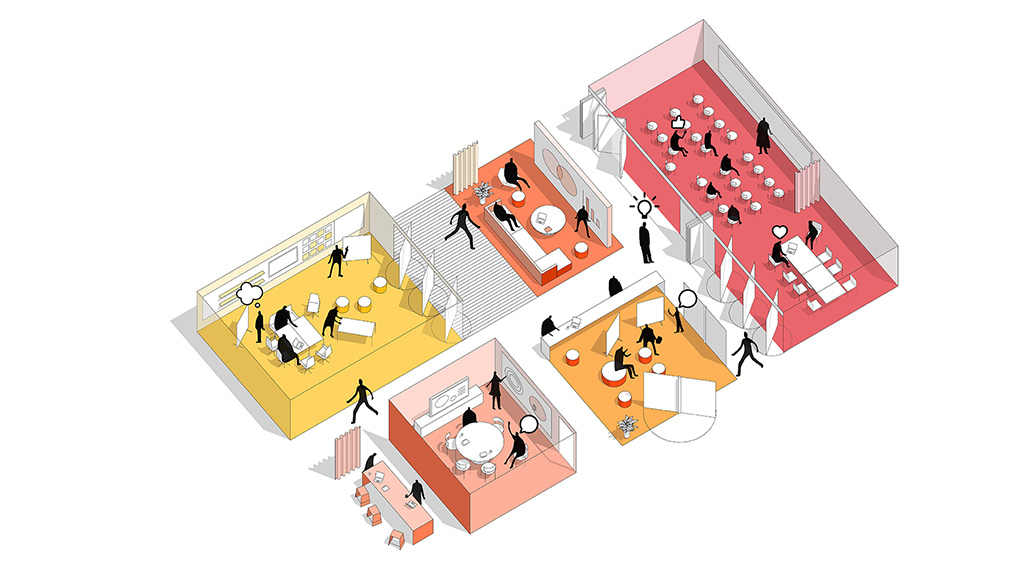
What Is the Future of Workplace Amenities?
The pandemic has been an opportunity for companies to rethink policies around employee flexibility and when — or if — certain job functions will return to the office. As the purpose of the office evolves, commercial office buildings will become even more amenity-centric.
November 06, 2020
|

What Does the Shift to a Hybrid Work Model Mean for Office Spaces in the U.K.?
We surveyed over 2,500 office workers across nine industries in the U.K. to learn more about their experiences working through lockdown and their expectations for the workplace once they return.
November 05, 2020
|

Why Curated Workflow Is Essential to the New Hybrid Workplace
As companies transition employees back into the new hybrid workplace, how do we get the right mix of people in the office at the right time?
November 04, 2020
|

Meeting Post-COVID Expectations for Office Buildings at One Post Office Square
Boston's 41-story One Post Office Square tower was constructed in 1980 and designed at a time when corner offices were the gold standard of the corporate workplace. When presented with the opportunity to reimagine the building, we aimed to bring in new life and identity, along with a revitalized experience both inside and out to position it as one of the city’s leading office towers.
November 04, 2020
|
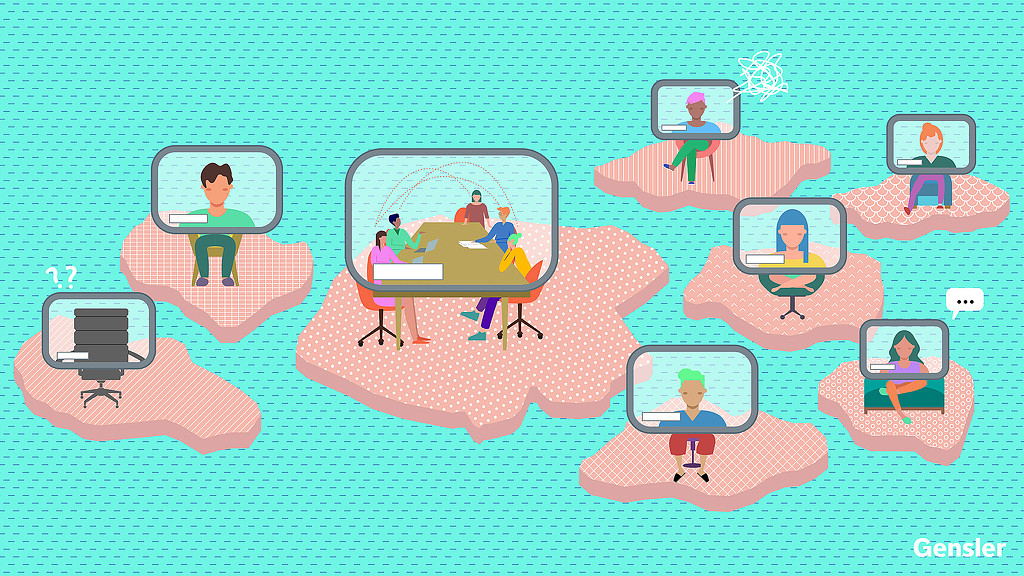
11 Considerations for Making Hybrid Meetings More Effective
When it comes to hybrid meetings, certain new etiquette is essential. Here are 11 considerations for making hybrid meetings more effective.
November 03, 2020
|

What Office Workers Want
The workplace is undergoing change, yes, but its relevance and centrality to the success of an organization remains.
October 30, 2020
|

What Gensler's City Pulse Survey Reveals About the Changing Urban Experience
Gensler’s City Pulse Survey 2020 findings provide developers, urban designers, and clients with real-time research into how the pandemic is impacting migration patterns, evolving expectations, and the urban experience across global cities, including New York, San Francisco, London, and Singapore.
October 28, 2020
|

Reimagining San Antonio as a 20-Minute City
The idea of a “20-minute city,” in which residents’ needs can all be found within a 20-minute walk or short bike ride from their homes, can be extended to cities across the globe.
October 27, 2020
|
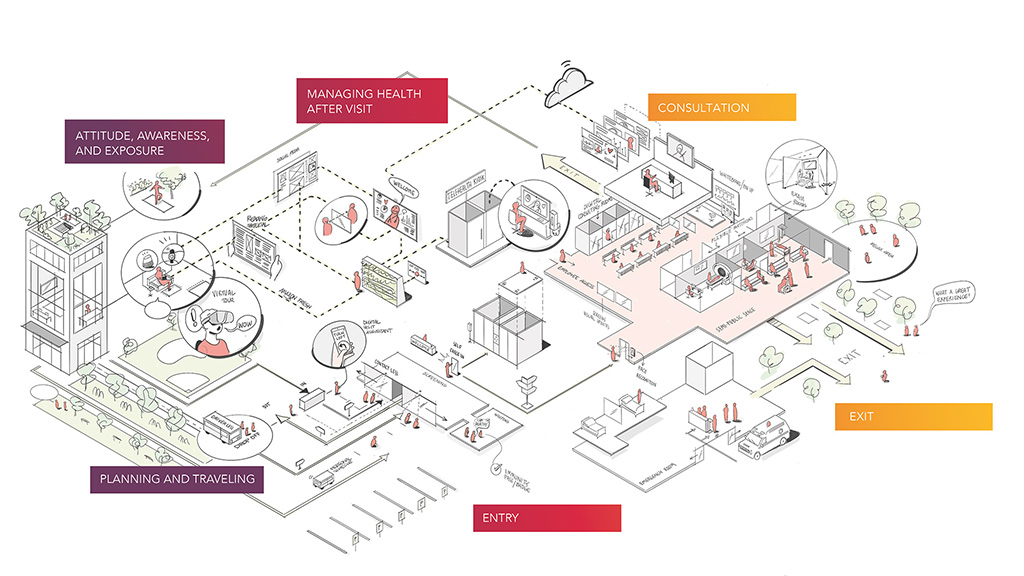
Where Have All the Patients Gone? The Art and Soul of Recapturing Lost Treatment Volume
To restore normal treatment activity in the long-term, healthcare delivery needs to take a more humane approach throughout all stages of the patient experience.
October 23, 2020
|

6 Strategies Developers Can Use to Improve Building Performance and Lower Carbon Emissions
A building’s performance is primarily influenced by its size, shape, orientation, massing, and fenestration. When just 1% of a project’s upfront costs are spent, up to 70% of its lifecycle costs may already be committed. Performance is first and foremost a design strategy.
October 21, 2020

The Future of Workplace Amenities Is Knowledge
As more businesses embrace flexible work, things like employee choice and well-being are taking precedent over the physical amenity spaces that employers companies once offered.
October 15, 2020
|

Design for the New Hybrid Workplace
As we plan for the new workplace, we need new design tools to meet the new design demands, and advances in technology and design tools is driving innovation with our clients in this space.
October 14, 2020
|

Assembly at North First: Putting Resilient Design to Work in the Wake of the Pandemic
Completed in 2019, Assembly at North First was originally intended to be leased as a single-tenant campus, but the developer asked Gensler to demonstrate what the post-COVID workplace would look like in practice.
October 14, 2020
|

How to Bring Older Office Buildings Back to Life Amid a Struggling Commercial Real Estate Market
Here are several opportunities commercial real estate developers can consider when converting or repositioning under-performing office buildings.
October 07, 2020
|

The Sustainable Hotel: Designing for Wellness and Resilience
In a world where there’s an increased focus on the impact we have on our planet, the travel industry is working towards green initiatives that enhance environmental wellness.
September 30, 2020
|

The Hospitality Industry Seeks to Reinvent Itself With the Adjacent Space
At the moment, everything we do has been dramatically upended, which is what has the hospitality industry rethinking its purpose. If the very meaning of work and home has changed, what does that mean for hotels?
September 30, 2020
|

Motel Revivalism: The Destination for Seamless Work & Travel
Tourists longing for road trips and outdoor adventures, paired with working travelers’ “work-from-anywhere" flexibility, can drive an opportunity to reimagine the nostalgic motel. Here are solutions to renovate existing motels or create a network of modernized motels that focus on wellbeing and fun, localized experiences.
September 30, 2020
|

Banks in Beta Mode: Repositioning a Place in the Community
There is no one-size-fits-all solution for reimagining the next evolution of physical banking locations, but it’s an opportune time for banks to re-evaluate and reposition their portfolios to help strengthen connections with clients and communities.
September 29, 2020
|
Digital Communications Tips for Workplace Reentry
Here are four best practices for digital communications when preparing employees for their reentry to the workplace.
September 24, 2020
|

The California Wildfires Are Yet Another Wake-Up Call for Resilient Design Strategies
Recent surges in wildfires and hurricanes are a wake-up call for climate action. Here are seven design strategies we can use to achieve climate resilience.
September 23, 2020
|

Creating Meaningful Content for the Built Environment
As digital experience designers, we design media architecture —or storytelling content — for a vast range of spaces to help curate the atmosphere within the built environment.
September 23, 2020
|

Are We Ready for the Heat? Desert-Appropriate Strategies for a Resilient City of the Future
As designers in this in an increasingly hot environment, we have the responsibility to lead by example and drive the effort in making Phoenix a resilient “City of the Future.”
September 22, 2020
|

Here’s How Developers Can Reposition Office Buildings for the Future
Office building developers can reposition tower blocks to create integrated, socially responsible buildings that contribute to the community and connect people.
September 16, 2020
|
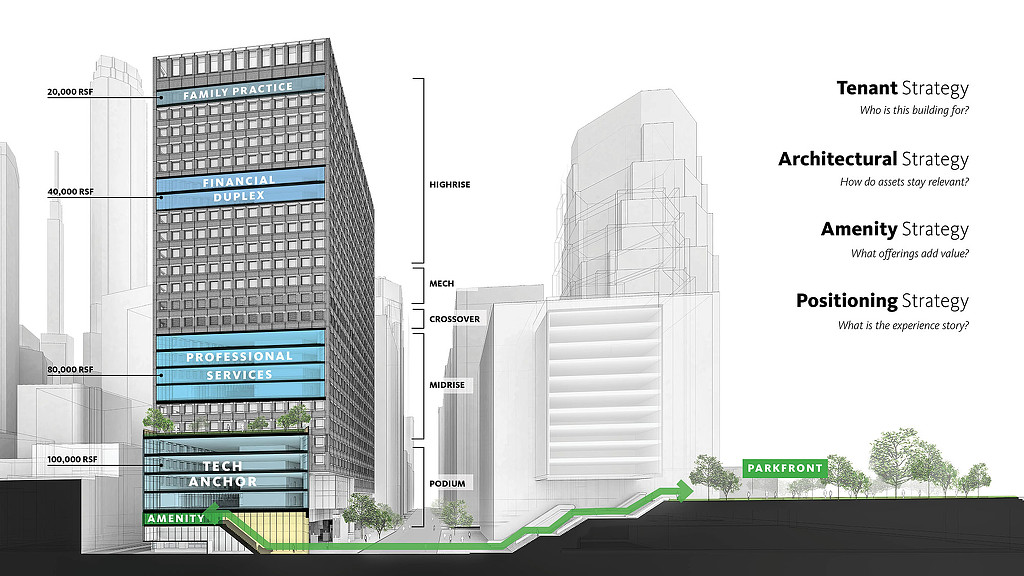
Real Estate Design Strategies for Leasing in a Post-COVID Market
Here are four key strategies that building owners and developers can leverage to have more informed conversations with prospective tenants in the post-pandemic market.
September 15, 2020
|
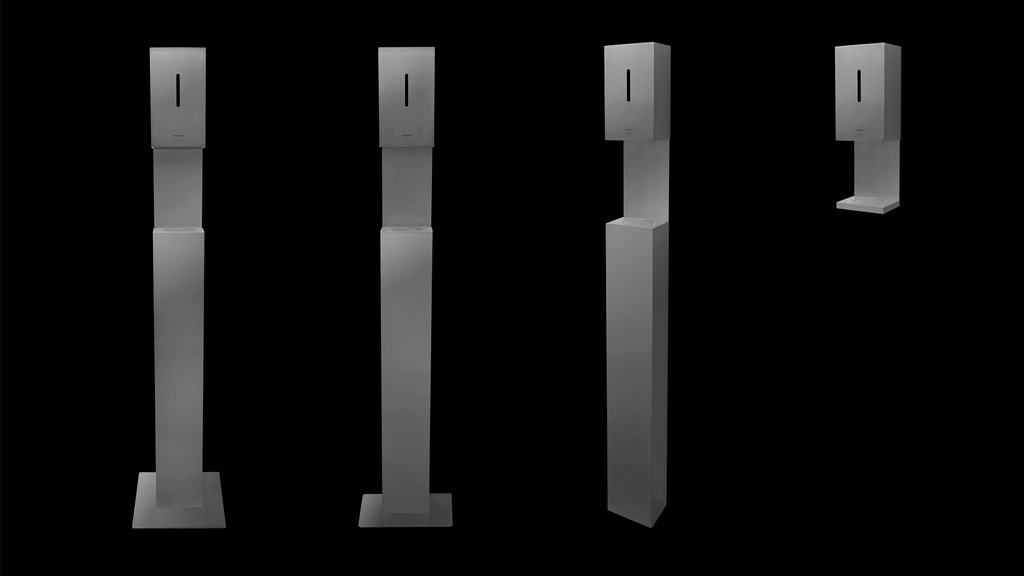
Product Design in Times of Crisis
Necessity really is the mother of invention, and full-blown crisis is especially effective for driving innovation.
September 09, 2020
|

How the Pandemic Has Shaped Our Understanding of the Trading Floor
Now that COVID-19 has challenged the norm, Gensler is examining how design should support trading floor activity.
August 31, 2020
|

How Workplace Design Can Ease Anxiety and Feelings of Isolation
Now that some workplaces are reopening, we’ll have to find a way to shake off these feelings in a world that remains very restricted. The question is how? And what role should employers play to support their people as they transition back to the office?
August 20, 2020
|
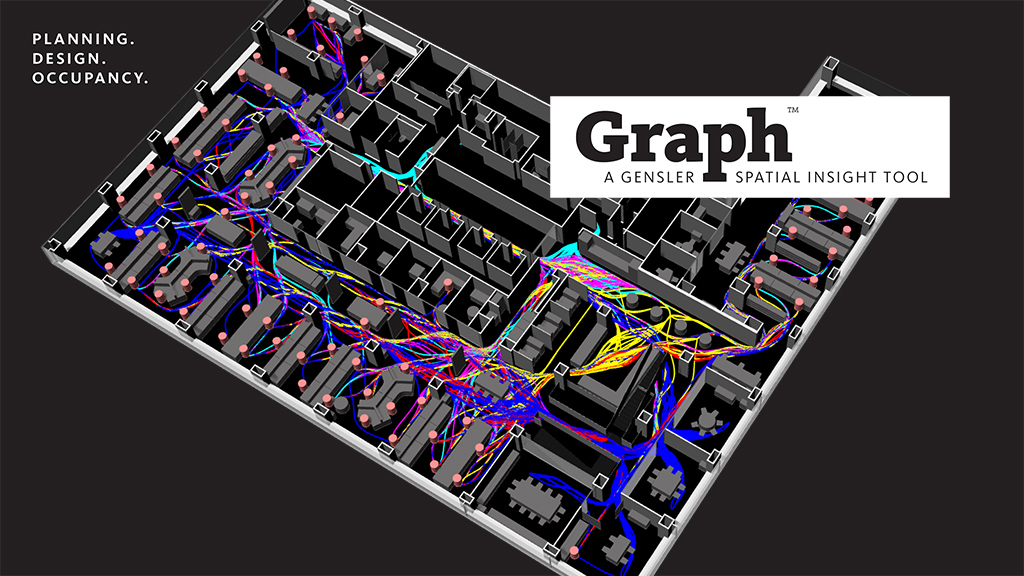
Graph by Gensler: Spatial Analytics for Design
Introducing an advanced spatial analytics service that reveals the impact of design choices, visualizes behaviors, and maps human experience to drive better outcomes.
August 12, 2020
|

The Office Building of the Future Should Be an Essential Part of Its Community
Over the past 70 years, the workplace has evolved slowly but surely. Now that evolution has accelerated far more dramatically and when we return, the office building is going to look and feel like a different place than the one we left.
August 05, 2020
|

A New Type of Tall Building Design for China
At nearly 500-meters high, Suzhou Zhongnan Center represents a new paradigm for tall building design and vertical living.
August 05, 2020
|

Design Ideas for the Post-Pandemic Public Library
Public libraries have long served as welcoming settings that offer community resources, but the pandemic challenged us to rethink the library experience.
July 28, 2020
|

COVID-19 and Building Performance: The Big Picture
From energy use to maintenance, lighting, and air quality, COVID-19 will change the equations we’ve been using to calculate the performance side of architectural design.
July 23, 2020
|

What 10 Million Square Feet of Data Tells Us About Social Distancing in the Workplace
Through our data and benchmarking, we’ve surfaced some key themes when it comes to social distancing in the workplace
July 22, 2020
|

Aiming for New Heights of User Experience With China’s Tall Buildings
As China continues to grow and many more people continue to move to cities, there must be a greater focus on the human experience of working, living, and playing in the urban environment.
July 20, 2020
|

Bringing Sports Back to the Venue
We’ve been working with our clients to understand the challenges, questions, and potential strategies to get players and fans back to the sports venue.
July 17, 2020
|

How Airport Design Can Restore Passenger Confidence
To get people flying again, the aviation industry needs to restore passenger confidence in the airport as an environment that protects passenger health and safety.
July 10, 2020
|

Reimagining a Safer, More Equitable Daily Commute
Here are four strategies to create a public transit commute that prioritizes people’s safety and equity.
July 08, 2020
|

How Tech Companies Could Benefit from a Decentralized Approach to Real Estate
Here are a few key considerations that tech companies might want to take into account as they reassess their real estate portfolio.
July 07, 2020
|

Are Our COVID-19 Responses Missing the Big Picture?
As we plan for a new normal, we must keep the climate costs of our post-COVID workplaces and consider how changes we make to deal with the virus might influence the climate.
July 07, 2020
|
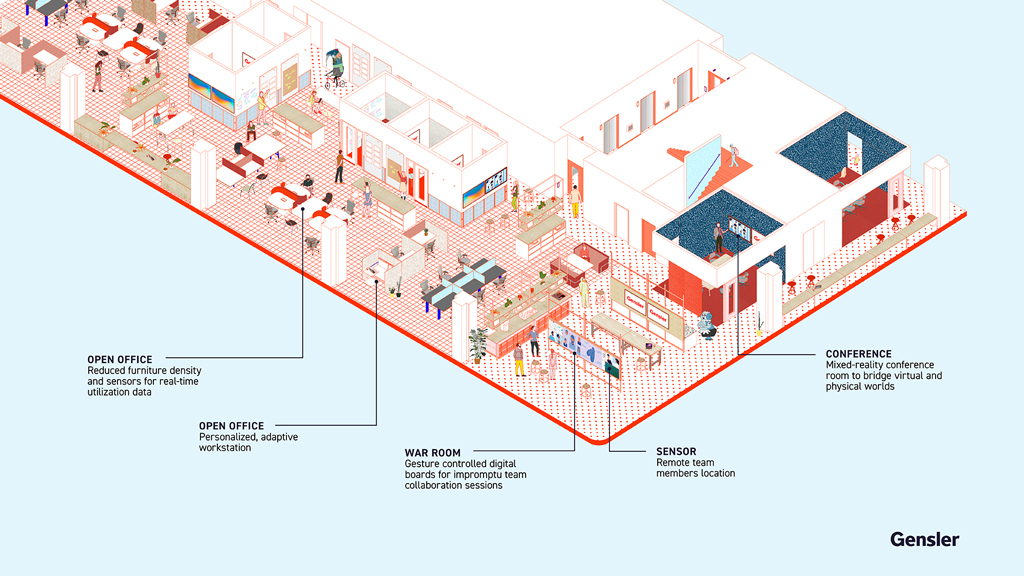
The Future Workplace Will Embrace a Hybrid Reality
We won't be returning to our former offices. Instead, the hybrid office might look similar in many ways, but it’s going to be strategically modified, incorporating new practices, new protocols, and new technologies to support hybrid workers.
July 02, 2020
|

Accessible Design for All in the Post-COVID Workplace
Here are some inclusive design strategies we can take to make the return to work accessible.
July 02, 2020
|

Reimagining the Future of Cities as Healthy Cities
Epidemics have shaped our cities for a long time. The key question in this moment is, how can we use what we’re learning to improve the quality of life in cities after COVID-19?
July 01, 2020
|

How the Pandemic Could Reshape the World’s Cities
We have an opportunity to provide a more fulfilling urban experience and to design for health, equity, and accessibility.
June 30, 2020
|

Rebuilding Consumer Confidence in Our Shopping Destinations
What are the long-term implications that will change how we experience shopping and leisure destinations?
June 24, 2020
|

4 Considerations for the New Retail Environment
How can retailers make customers feel engaged and at ease as we emerge from these challenging times?
June 22, 2020
|

Designing Spaces to Help People Feel Emotionally Safe in the Workplace
How can we help people feel emotionally safe when they venture outside their own homes and interact in public or private spaces?
June 19, 2020
|

Return Strategies Must Prioritize Mental Health and Resilience
Organizations must communicate with empathy and develop strategies that put mental health in lockstep with physical health and safety for their employees.
June 18, 2020
|

Crafting Our Way Into a New Era of Human Connection
With all the talk about re-entry, return to work, and reopening of retail and schools, it seems the measures the world is taking to welcome people back are somewhat in conflict with our longing for community and connection.
June 16, 2020
|

What Will the ‘New Normal’ for Automotive Retail Look Like?
The response to Covid-19 has sparked rapid change by automotive manufacturers and retailers to satisfy the needs of the market.
June 08, 2020
|

Fusing Architecture and Technology to Reenter a New World
As we emerge from lock-down, we are all wondering what it’s going to be like to reengage with the spaces and places in our communities. What new world are we entering into?
June 08, 2020
|

The Near Future of Casino and Gaming Design
Here are some insights that could have implications for gaming environments in Las Vegas and around the nation.
June 01, 2020
|

What Matters Most for Hospitality in Asia Pacific and the Middle East?
These are difficult times, but travel will resume and we recognize that great hotels not only anticipate market changes, but they are also able to react quickly to unusual situations.
May 29, 2020
|

Why Today’s Universities Need to Be Global Institutions
How can universities mitigate a potential downturn? The answer is transnational education.
May 28, 2020
|
6 Considerations for Transitioning Back to School
Here are some tools and considerations to guide academic institutions in transitioning back to campus.
May 28, 2020
|
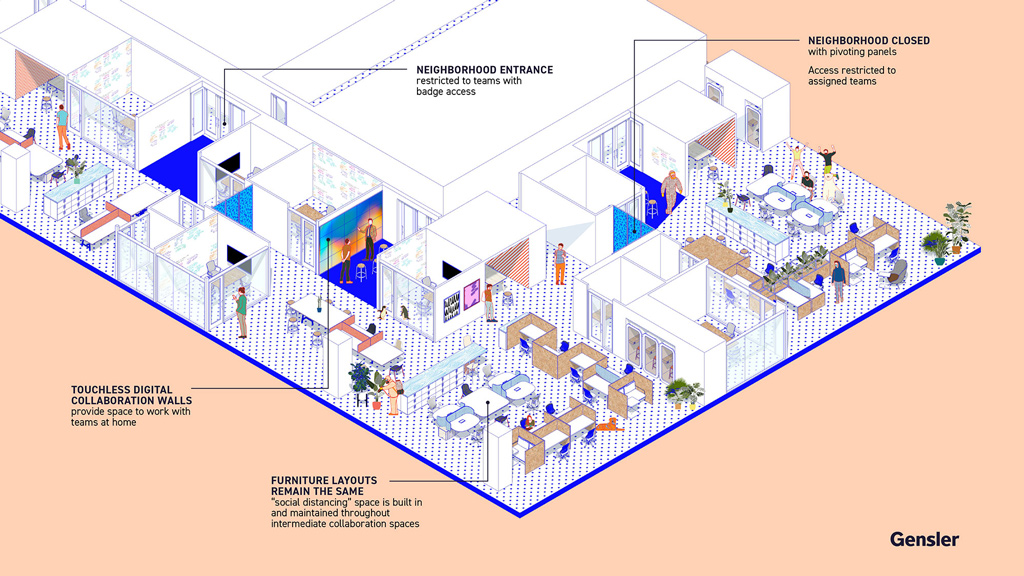
Reports of the Death of the Workplace Have Been Greatly Exaggerated
For millions of office workers around the world, work has been consciously uncoupled from its usual location for the first time. No doubt, the offices we return to will evolve along with changes in business priorities and cultural norms.
May 27, 2020
|

Community Impact Is a Key Strategy in Returning to the Office
Community impact has the potential for positive, long-lasting benefits on our workforce and our culture.
May 27, 2020
|

Insights From Gensler’s U.S. Work From Home Survey 2020
The Gensler Research Institute published its U.S. Work from Home Survey 2020, featuring findings on the experience of working from home during the pandemic and insights on how this experience is influencing people’s expectations for the future workplace.
May 26, 2020
|

Transitioning to a Virtual World of Health & Wellness
The landscape of virtual care has leapt ahead a decade or more amidst the current health crisis, and it is creating a massive shift in operations at a time when a historic financial decline has hit the healthcare industry.
May 22, 2020
|

Most People Want to Return to the Office — But They Expect Changes
We’ve proven we can easily and efficiently work from home. But we can’t effectively do all work activities from home. In fact, the workplace may be more important than ever moving forward.
May 22, 2020
|

How Companies Can Support Work-From-Home Best Practices in the Long Term
As businesses eye a strategic and safe return to the office, here are the operational mechanisms they should consider in order to support partial working from home on a permanent basis.
May 22, 2020
|

A Day in the Life: Going Back to School in China
Here’s what we've learned from our colleagues in Gensler’s Shanghai office about school reopenings in China.
May 19, 2020
|
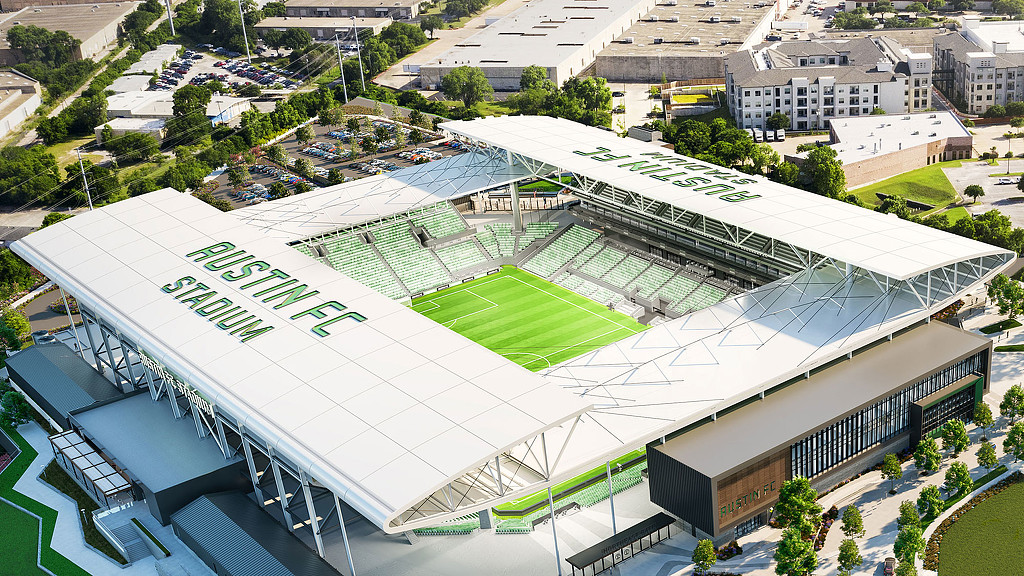
Is the Virtual Fan Experience Ready for the Big Game?
Until fans are allowed back inside sports arenas, what can we do now to enhance the fan experience virtually?
May 18, 2020
|

Resilient Cities Rely on Resilient Food Systems
The pandemic is challenging food supply chains. Implementing intelligent urban agriculture can enhance resilience and food security worldwide.
May 15, 2020
|

What Going Back to School Might Look Like
What does the future of education look like, and what should schools be doing now to prepare?
May 14, 2020
|

The Future of Dining Out
Here are six considerations for restaurant and bar owners in an era of new consumer expectations.
May 14, 2020
|

How to Design Hospital-Ready Hotels
The current pandemic has proven that hotels can play a variety of essential roles in times of crisis.
May 13, 2020
|

Will There Be a Climate Change Vaccine?
We didn’t have a warning of the COVID-19 crisis, but we do have a warning for the climate crisis up ahead.
May 11, 2020
|

It’s Time to Rethink Signage and Wayfinding for Transportation Hubs
Fast forward to when you’re ready to take your next flight. When that day comes, what’s it going to take to make you feel safe?
May 11, 2020
|

Designing Government Offices for the Post-COVID Era
As we prepare to return to the workplace, whenever that happens, what should public agencies and departments be doing to prepare a workplace that can help people feel healthy?
May 11, 2020
|

Defining the Future of Our Cities: Five Areas of Opportunity for a Post-Pandemic World
We are witnessing global disruption at an unprecedented scale. But if we can live though disruptions, then we may emerge even stronger and more resilient as a community.
May 08, 2020
|
Tips for Signage and Wayfinding in a Post-COVID-19 World
Signage and wayfinding graphics can introduce healthy practices and help people feel at ease in this time of uncertainty.
May 06, 2020
|

As Data Demand Surges, It’s Time to Invest in IT Infrastructure
The demand for data spurred by this health crisis has highlighted the need to invest in critical facilities infrastructure.
May 06, 2020
|

How Will Hotels Rebound from COVID-19?
Seven key considerations that will change how we travel and experience hotels.
May 05, 2020
|

Giving Back Has Never Been More Important
In this time of crisis, we need to double down on our community impact efforts.
May 05, 2020
|

An Architecture of Optimism for a Post-Pandemic Society
Whether it’s new buildings that are about to be designed or existing architecture that now needs to be re-imagined, in many ways this is a time for an architecture of optimism – one that promotes wellness and celebrates life.
May 04, 2020
|

Sharing Our Work-From-Home Experience in Asia Pacific and the Middle East
After Gensler staff members in the Asia Pacific and Middle East region began working from home, we launched a survey to assess our people’s well-being, challenges, and overall experiences — here are key findings.
April 30, 2020
|

An Air Filtration Primer for Building Owners and Developers
Here are key changes we need to make to the built environment in order to provide spaces where people can feel safe as they return to work.
April 30, 2020
|

New Opportunities for Mobility Amid COVID-19
Our wholesale shift in live-work-play behaviors as a result of COVID-19 have provided us an opportunity to rebalance public rights-of-way.
April 29, 2020
|

For Law Firms, COVID-19 Has Accelerated the Inevitable
The overnight shift to working from home is upending the model of how much real estate law firms really need.
April 29, 2020
|

Will the Work From Home Trend Impact Residential Design?
As working from home gains acceptance and more remote roles are fulfilled, the fundamental principles of workplace design will still apply — just in a residential context.
April 28, 2020
|

What We Can Learn From the Energy Industry About Safety in the New Workplace
The energy industry's safety practices can be adopted by many to cultivate a culture that prioritizes safety and wellness.
April 28, 2020
|

Planning for a Post-COVID Return to Campus
We're reflecting on the factors education leaders should consider in planning a return to school post-COVID-19, and what we can learn from this remote learning experience to create a resilient hybrid campus.
April 23, 2020
|

How Should Office Buildings Change in a Post-Pandemic World?
For those who design and develop office buildings around the world, the current crisis has introduced a new challenge: Once we are cleared to return to the office, how can we convince people that the buildings they use are healthy and safe?
April 23, 2020
|

Brand Experiences Must Be Human Experiences
We’re telling different stories today — stories of isolation, but also of newfound connection.
April 22, 2020
|

A Day in the Life: Going Back to Work in China
As the COVID-19 pandemic continues, in China we are slowly experiencing going back to work. Here’s what we learned during our return to Gensler’s Beijing office.
April 22, 2020
|

Could Low-Tech Design Prevent Climate Change-Influenced Pandemics?
How should we think about the coronavirus pandemic in the context of climate change? Is there anything we can do differently in the built environment to fight these two urgent problems?
April 21, 2020
|

Understanding the Touchless Workplace
In the workplace, digital solutions and experience platforms have improved guest check-in, conference room booking, company communications, wayfinding, food and beverage service, and more. But touch-based solutions start to look like health risks in light of the recent pandemic and other viral threats.
April 15, 2020
|

Redesigning Mixed-Use Environments for a Post-Pandemic World
What will mixed-use and public places look like after this pandemic?
April 15, 2020
|
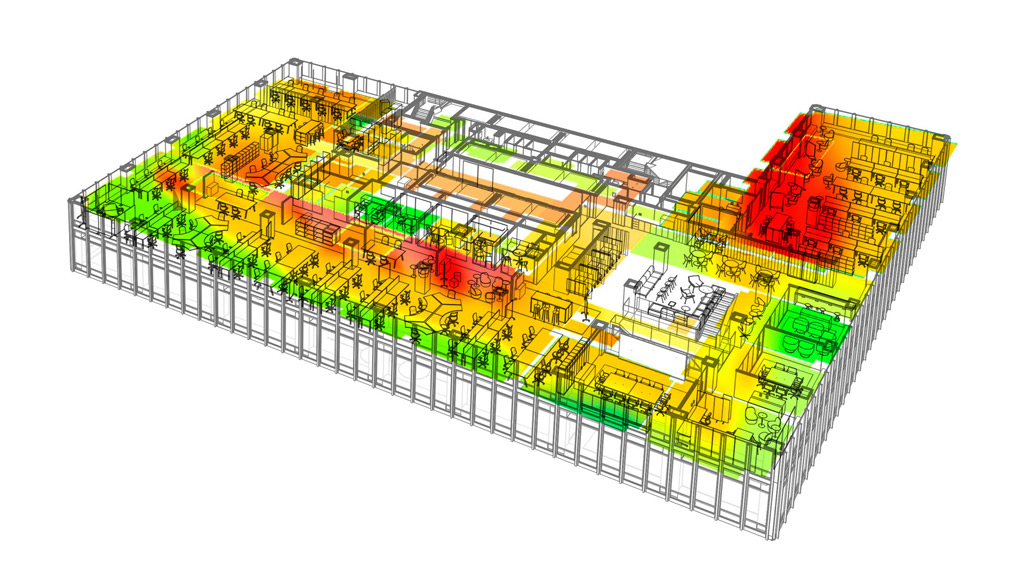
Creating Data-Rich Workplaces to Detect and Curb Viral Transmission
Workplaces can be optimized to collect population data — like thermal screening — so agencies and companies can make better informed decisions to protect the wellness of their people.
April 15, 2020
|

Taking Care of Each Other in the Post-Pandemic Open Office
Once we return to the office, we’ll need to transpose our newly discovered sense of community accountability back into the workplace.
April 10, 2020
|

How the Pandemic Can Lead to Better Public Meetings
Public meetings are the foundation of modern participatory democracy. So, what do we do when it’s dangerous or impossible to gather people in public places? How should governments respond now and in the future?
April 10, 2020
|
Fostering Casual Collisions — and Creativity — in a Virtual World
Some of the best ideas at work happen spontaneously — in the lunch line or waiting for the elevator — rather than in a conference room. Now that many of us have shifted to working 100% virtually, how do we continue to create opportunities for casual collisions that spark ideas and random discussions?
April 07, 2020
|

Re-Entry for Retailers: Returning to the Store
Retailers can start formulating a plan for re-entry that meets consumers' new expectations of the marketplace.
April 06, 2020
|

What Happens When We Return to the Workplace?
It’s not too early to start planning how we can return people to the workplace once the COVID-19 crisis ends.
April 03, 2020
|

Using This Moment to Improve City Life
The current crisis raises serious questions that we’ll need to address before we get back to anything resembling normal: How well-suited are cities to a post COVID-19 world? How prepared are we to handle a health crisis in the future? And how can we use what we’re learning now to improve the quality of life in cities?
April 03, 2020
|
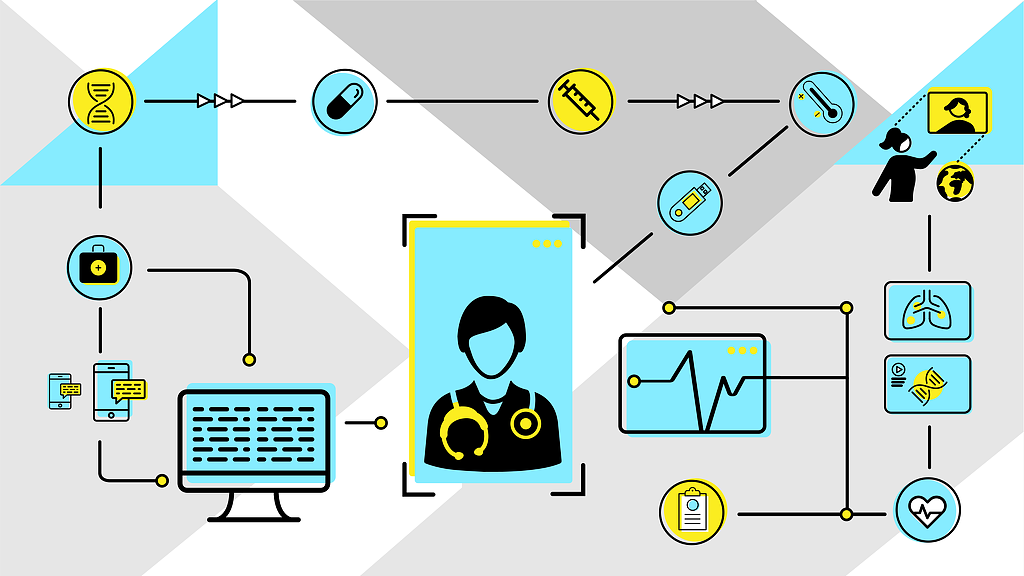
The Pandemic’s Lasting Effect on Our Healthcare System
After this crisis, we won’t return to business as usual. What should we consider as the new normal for healthcare systems?
April 02, 2020
|
Will Campus Life Translate to a Virtual Environment?
COVID-19 has forced us to embrace a new reality rooted exclusively in virtual interactions. While we reflect on how educational institutions’ responses are leading to a paradigm shift in the learning experience, how might campus life also translate to a virtual experience?
April 01, 2020
|
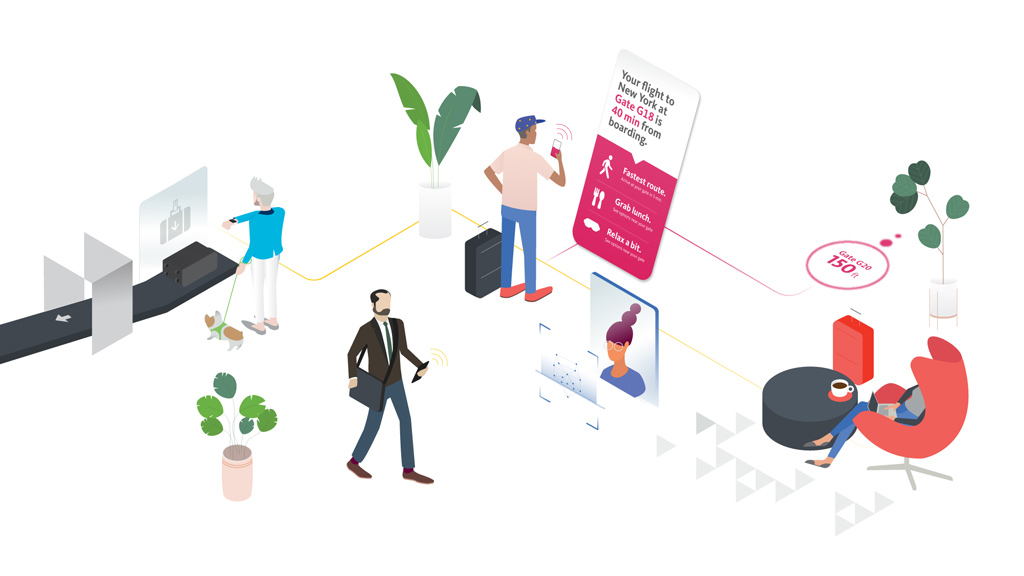
Airports Are Facing a New Reality
In the wake of the COVID-19 pandemic, we’re thinking about what airports can do to save the air travel industry and regain passenger trust.
March 31, 2020
|

Redefining Wellness in the Face of Pandemic
The COVID-19 crisis is causing us to redefine all our work around the concept of wellness and re-examine the importance of resilience.
March 30, 2020
|
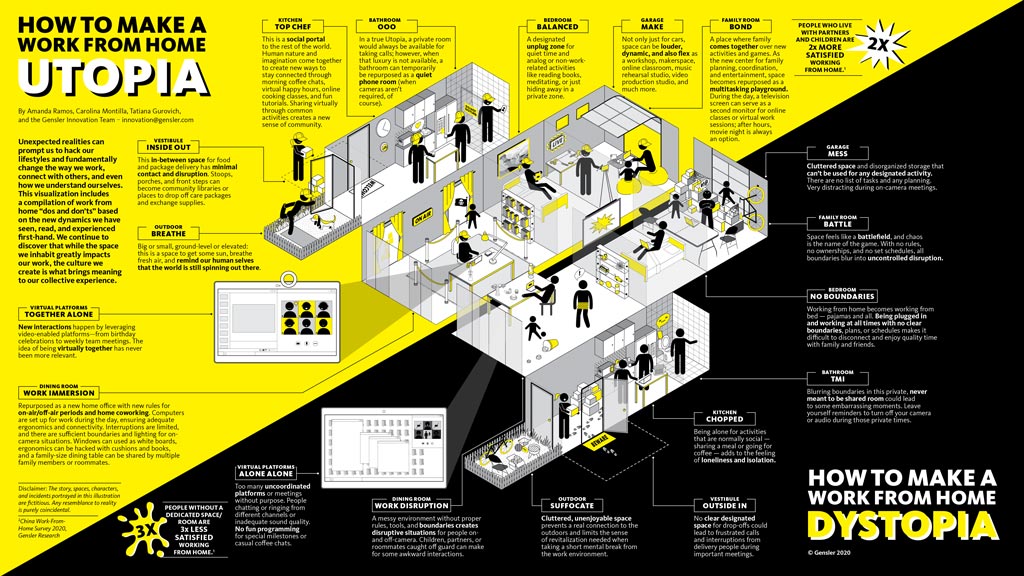
How to Build Culture
in a Virtual World
As COVID-19 causes the world to rethink the communal workplace, for businesses it’s also a philosophical and emotional assault on company culture.
March 26, 2020
|

Digital and Virtual Connections Have Quickly Become a Brand’s Livelihood
In this time of social distancing, brands are finding new ways to authentically connect with their audiences through digital and virtual experiences.
March 25, 2020
|
Designing Healthcare for Surge Capacity
We need health and wellness systems that continue to give people more choice and we need those systems to flex and respond to pandemics like COVID-19.
March 23, 2020
|

Remote Working Offers an Opportunity to Experiment and Learn
As COVID-19 disrupts our lives, working from home is now a sudden reality. How can we apply the best practices and tools that make a corporate workplace effective and collaborative, and instead create a great work from home space and routine?
March 18, 2020
|

We Are in the Midst of a Paradigm Shift for Higher Education
As we make short-term decisions to respond to the global pandemic, we will also have a long-term opportunity to reinvent the traditional university learning experience.
March 17, 2020
|

Designing Office Building Lobbies to Respond to the Coronavirus
People spend up to one-third of their lives at work, many of them inside office buildings. If these buildings were proactively designed with features that could stem the spread of communicable disease, the wellness benefits for the general workforce could potentially be widespread.
March 13, 2020
|

Envisioning a Future for USPS Real Estate
As the largest retailer in the nation, the United States Postal Service is uniquely positioned to shape the future of communities across America.
March 05, 2020
|

Design Forecast Denver: Shaping the Future of Our City
Gensler Denver hosted a discussion about challenges facing cities such as affordable housing, mobility, and climate change.
March 05, 2020
|

Future Cities, Future Buildings
The Johnson Controls (JCI) Asia-Pacific Headquarters in Shanghai, China is a case study in designing and engineering super progressive environments.
March 02, 2020
|

Creating Meaningful Customer Relationships in the Midst of a Merger
A merger has a profound impact on customer experience, but also provides an opportunity to re-focus on what’s working for customers and how best to target and serve new ones.
February 28, 2020
|

Design Forecast Costa Rica: Shaping the Future of Cities Through the Human Experience
Gensler Costa Rica hosted a panel discussing how public-private partnerships can spur innovation and how buildings and districts are key components of successful cities.
February 25, 2020
|

Design Forecast Charlotte: Designing for the Displaced
Gensler Charlotte hosted a discussion about critical issues of affordable housing and homelessness facing our community.
February 25, 2020
|

Design Forecast Washington, D.C.: Resilience in Our Region
Gensler’s Washington, D.C. office hosted a hyperlocal conversation focused on what the resilience challenge means for the community, and possible solutions.
February 19, 2020
|

Experiential Design is Changing the Rules of the Workplace
Client insights from Gensler Morristown's panel discussion on workplace performance.
February 14, 2020
|

Design Forecast Detroit: Shaping the Future of Cities
Gensler’s Detroit office hosted a discussion on urban innovations and their impact on the future of a mobile, connected, and inclusive Detroit.
February 11, 2020
|

Flexible Workspace is on the Rise in the U.K.’s Corporate Sector
Gensler paired up with the British Council of Offices to find out what’s driving the rise of flexible workspace in the U.K. corporate sector.
February 04, 2020
|

Want Your Organization to be More Creative? Embrace these Four Workplace Strategies
Today, encouraging creativity is a must in every business, from law firms to banks to media companies. A creative culture can come from many factors — but the space you house it all in can be a huge amplifier of creativity.
January 28, 2020
|

Developing the World’s Tallest Net Zero Timber Building with Sidewalk Labs
Working with Sidewalk Labs, engineers, environmental specialists, and partners, we explored timber’s potential impact on building design, manufacturing, and sustainability.
January 24, 2020
|

The Benefits of Inadvertent Knowledge Transfer
We often learn by overhearing our peers and experiencing the consequences of their behavior — positive, negative, and everything in between — in real time, in person. This is just as true for the workplace as it is for childhood education, and it is just as relevant for factual information as it is for life lessons.
January 15, 2020
|

Gensler Design Forecast Tokyo: How to Win the Battle of Workstyle Transformation
Gensler’s Tokyo office hosted a workshop on how to create a smart and balanced workplace, and investing in the right amenities to attract and retain top talent.
January 15, 2020
|

Blank Canvas: Using Art to Create Community in the Workplace
Whether it is a curated art program, an emerging artists installation, or a dedicated gallery, organizations are finding unique ways to use art as a tool to inspire social change and connect with the community.
January 13, 2020
|

Design Forecast Toronto: The Future of Cities
Gensler’s Toronto office hosted a series of presentations that showcased potential futures and near-term solutions for shaping the future of cities.
December 20, 2019
|
Design Forecast Newport Beach: Shaping the Future of Orange County
Gensler’s Newport Beach office hosted a panel discussion on topics ranging from mobility to interconnected communities, social impact, and climate change.
December 20, 2019
|
Design Forecast Newark: Designing Cities for People
Gensler’s New Jersey office hosted a panel discussion on topics ranging from social equity, to new modes of mobility, and the importance of placemaking in economic development.
December 20, 2019
|

Design Forecast Dallas: People-Centered Workplaces Are Driving Connected, Resilient Cities
Gensler Dallas hosted a panel discussion exploring global trends in workplace and office building design, and how the human experience is the driving force behind more resilient, connected cities.
December 13, 2019
|

Cal-Australia Dreamin’
Addressing the realities of climate change through aspirational policy.
December 13, 2019
|

Design Forecast Las Vegas: Shaping the Future of Work
Gensler Las Vegas hosted a conversation on topics such as top office amenities, branding and identity, and how balance and choice drive the most effective and engaged workplaces
December 12, 2019
|

Design Forecast La Crosse: The Future of Work
Gensler’s La Crosse office hosted a panel discussion on workplace trends, including tips for connecting a mobile workforce and managing change in the workplace.
December 10, 2019
|

Schooling Kids in the Power of Design
Our long-standing partnership with City Year aims to transform educational spaces with heart for the next generation.
December 09, 2019
|

AI is Transforming Workplaces. What Does That Mean for Law Firms?
For law firms around the world, artificial intelligence could have seriously impactful possibilities that shape how legal services are delivered in the future, as well as what types of services lawyers could offer.
December 05, 2019
|

Designing Intergenerational Communities
In partnership with the Milken Institute's Center for the Future of Aging, Gensler created speculative designs to show how multigenerational communities can be achieved in existing urban environments.
December 03, 2019
|

Singles’ Day: From Service to Experience Economy
What started as an informal celebration among Chinese university students has evolved into the single biggest shopping day worldwide — both online and off. How are traditional retailers and e-commerce behemoths in China using digital platforms and physical space to create authentic and lasting connections with consumers in the midst of these mind-boggling sales figures?
November 25, 2019
|
Design Forecast Houston: Our Role in Our City’s Future Experience
Gensler Houston hosted a panel to discuss topics ranging from mobility, to climate change, and the future of livability in Houston.
November 25, 2019
|

Design Forecast Philadelphia: Creating Innovative Workplaces to Attract (and Keep) the Best and the Brightest
Gensler Philadelphia hosted a panel on the future of workplace discussing key topics such as emerging technologies, talent competition, and the experience economy.
November 22, 2019
|

Microsoft’s New U.K. Flagship: A Vibrant Community Hub
The tech company's first European flagship is more than just a place to shop or demo products — it’s a destination to engage with the local community and connect with all types of people — from gamers and students, to educators, families, and businesses.
November 21, 2019
|

Resilient Cities Begin With Resilient People
Gensler's Denver office partners with Access Gallery, whose mission is to create community and nurture creativity among young adults with disabilities.
November 18, 2019
|

Design Forecast Singapore: Repositioning for Smart Cities
Gensler Singapore hosted a panel examining the impact that repositioning smart cities might have on a well-established, dense urban environments.
November 13, 2019
|

Emotional Security in the Workplace
Creating an environment where employees feel empowered to take risks, ask questions, pose new ideas, and fail can be more important than the environment itself.
November 07, 2019
|

Design Forecast Bay Area: Shaping the Future of Connected Cities
Gensler's San Francisco Bay Area offices hosted a panel discussion on new strategies being used to shape the future of the Bay Area and the responsibilities we have to this unique landscape.
October 23, 2019
|

Embracing Constraints to Build a More Sustainable Shanghai
The composed elegance of the 60-story One Museum Place in Shanghai's Jing'an District tells a story of breathtaking skill and ingenuity amidst complex urban limitations.
October 18, 2019
|

Design Forecast Charlotte: Tech Talent in the Queen City
Gensler Charlotte hosted a discussion about the future of work and how the it will shape human experience in the city, covering topics such as the tech gender gap and the war for talent.
October 18, 2019
|

Design Forecast Phoenix: A New Workplace Narrative
Gensler Phoenix partnered with our local ULI chapter to bring the local community together to discuss new challenges in workplace design, from coworking to change management.
October 14, 2019
|

The Future of Climate Policy Starts in Our Cities
Densely populated urban areas are epicenters for greenhouse gas emissions, but the policies made by local legislatures are informing global solutions to climate change.
October 08, 2019
|

Celebrating 20 Years of Design Excellence
The Gensler Design Excellence Awards is a program that seeks to elevate the firm’s design quality and celebrate design excellence in our projects.
October 03, 2019
|

Hospitals in an Age of Climate Change: Can They Survive the Storm?
In the face of extreme weather events, we must plan and design healthcare facilities that can assure quality care even when other basic infrastructure fails.
September 26, 2019
|

Doubling Down on Our Commitment to Resilience
With hundreds of millions of square feet of buildings and interior design projects in the pipeline annually, we believe our impact and role in reducing energy demand is critical. That's why we're announcing the Gensler Cities Climate Challenge with an ambitious goal for the entire design industry: eliminate all greenhouse gases associated with the built environment.
September 20, 2019
|

A 'What If?' Manifesto: Improving the Bus Experience
In the U.S., subpar bus riding experiences are common. While that may not be everyone’s daily bus reality, it raises the question: what if this were different?
September 17, 2019
|

The Inertia of Home
For tenants, moving is expensive and time-consuming. For owners, high turnover is costly. How do we create an “inertia of home” that entices people to truly come to rest?
September 12, 2019
|

Enlivening a Dead Block in San Jose
With the city's support, Gensler San Jose helped repurpose the ground floor of an uninviting parking garage to accommodate micro-retail spaces for local business owners, enliven the community, and encourage a renewed pedestrian experience.
September 05, 2019
|

Transforming Walmart’s Home Office in Bentonville
The world’s largest retailer’s new home office is a connected and sustainable campus where associates are inspired to do their best work.
August 27, 2019
|

Healthcare Providers Take Note: Every Space is a Healthy Workspace
As more organizations provide active, healthy workplaces, healthcare providers are following suit and discovering how a well-performing workplace can be beneficial for everyone.
August 26, 2019
|

In Africa, Your Solar Panels Don’t Mean Squat
The idea of sustainability, as we currently understand it, just doesn’t hold for the developing world.
August 16, 2019
|

Creating an Organizational Appetite for Sustainable Design
As people’s attitudes towards sustainability evolve alongside new modes of working, there is a real need for organizations to be intentional about how they implement any new changes.
August 06, 2019
|

Growing Biopharma Trend: Putting Science on Display
In the highly competitive research landscape centered around New Jersey, biopharmaceutical companies are aligning these values by moving the laboratory front and center, and putting their science on display.
July 25, 2019

Did Your Building Grow With BOMA 2017 Office?
Developers, landlords, and building owners have been adding balconies, patios, and other outdoor amenities to keep up with tenant demand, but the trend is creating challenges.
July 23, 2019
|

10 Key Design Interventions for a Healthier, Happier, and More Productive Workplace
Healthy, happier people are more productive, more likely to collaborate, and more likely to innovate in ways that benefit the bottom line.
July 12, 2019
|

A Multi-Stakeholder Approach to Tackling Rural Waste Management
On Isla Chira, a remote island in Costa Rica's Gulf of Nicoya, a recent groundbreaking showcases Gensler’s commitment to both the environment and making significant local impact.
July 02, 2019
|

Managing for Creativity
To keep up with the robust pace and dynamics of our environment, every organization needs to creatively innovate while delivering value to the bottom line.
June 28, 2019
|

Designing the Unexpected
Gensler San Francisco gathered a diverse panel of experts to consider the questions we should all be asking ourselves: does city life make us happy? Are our anxiety levels increasing? Are we starving for more human connection?
June 27, 2019
|

Building a More Inclusive University Environment
Small universities are having a hard time providing physical space for their diverse student populations. These campuses are often landlocked and lacking the enormous budgets of some of their larger counterparts. This raises the question: how can smaller universities support inclusion at a small scale while yielding a large impact?
June 25, 2019
Design Forecast Atlanta: Every City Has a Brand
A city's brand originates from the people who make its neighborhoods rich with personality, values, and promises. Each of us is a brand ambassador for our city, and collectively we create shared experiences that define who we are, and who we want to be.
June 21, 2019
|

Designing Informal Learning Environments with 826 National
826 National, a not-for-profit creative writing and tutoring center network serving underprivileged youth, is taking a novel look at designing learning spaces.
June 20, 2019
|

Community Engagement in Motion
The projects that are most successful are often the ones that invest time in the community and build something greater together.
June 17, 2019
|

Designing a New Platform for Uber's Vision of Aerial Rideshare
The vision of aerial ridesharing presented at the 2019 Uber Elevate conference this week is a bold one that promises to shift the way people experience cities — and one that will be a reality much sooner than most people think.
June 12, 2019
|

Community Impact Puts People First
At Gensler, we put people first. Nowhere does that shine through stronger than in our strategic model for Community Impact.
June 12, 2019
|

Hospitals Are Moving Into Their Communities
In the healthcare industry, provider loyalty no longer comes from proximity alone. Thanks to a global trend of digitalization and increasingly available medical knowledge, healthcare consumers are now empowered to seek out providers that offer greater levels of accessibility, convenience, and service.
May 31, 2019
|

California’s New Gold Standard for Net Zero Developments
California’s new Zero Net Energy code revisions will drive the creation of perhaps the greatest concentration of energy efficient buildings on the planet.
May 24, 2019
|

Creating Space for Mental Health Conversations in the Workplace
Work can be both a source of — and a relief from — the stresses of modern life.
May 17, 2019
|

The Promise of the Internet of Things in an Airport Environment
In the competitive scramble of airlines and airports to differentiate themselves, the Internet of Things has wide-ranging potential to improve operations and enhance the traveler experience.
May 10, 2019
|

Just a Government Town? Think Again.
High-profile tech companies and consumer brands are relocating to Washington, DC. And they’re not coming for the usual Washington reason: to be near the Federal government.
April 29, 2019
|

The Power of Narrative in an Era of Evolving Legacies
With boundaries between media and technology constantly blurring, it is easy for media companies to lose sight of both their own legacy and the narrative they seek to craft. At the WTOP headquarters in Washington, D.C., however, a clear, purposeful celebration and expression of brand legacy stems this tide. When a story of this nature is told through workplace design, the results can be extremely powerful not only for employees, but also curious guests or clients.
April 25, 2019
|

Designing a More Flexible, Healthy, and Expressive Legal Office
When it comes to recruitment and retention at law offices, it’s no longer enough just to have a workplace that functions well. A workplace has to capture and enhance a firm’s culture through a variety of design approaches.
April 23, 2019
|

Urbanism and the Pursuit of Happiness
Cities are magnets for those who seek better jobs, opportunities, and more diverse communities. But does city life make us happy? We look at some of the basic building blocks for a better, happier city.
April 18, 2019
|

Houston's ByDesign Group Explores Local Ideas for the Future of Cities
A group of young architects and designers at Gensler Houston are proposing big, bold ideas for the future of their city and beyond.
April 16, 2019
|
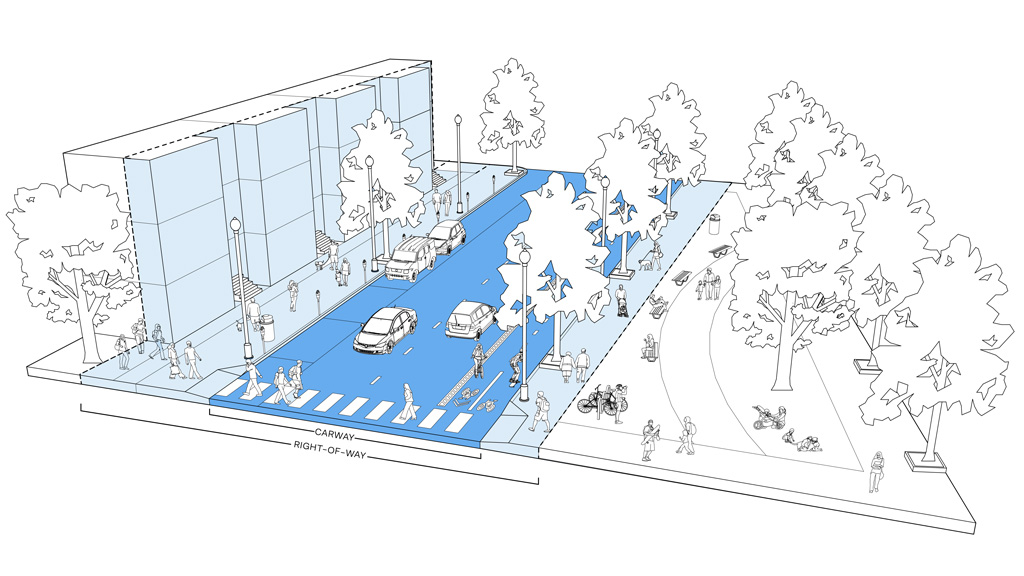
A How-to for Creative Placemaking and Tactical Urbanism
Pop-up, temporary, and semi-permanent public space projects have evolved past being mere experiments. They now form a substantial part of urban business operations that governments and developers are championing, but until recently policies around temporary use of the urban realm have been murky and difficult to navigate.
April 11, 2019
|

You Are Beautiful: Dining by Design
For the 22nd installment of DIFFA New York’s Dining By Design, design firms across the city mobilized to produce 23 carefully curated dining vignettes that raise awareness for individuals impacted by HIV/AIDS. Gensler New York’s 2019 design concept, titled “You Are Beautiful,” served as a celebratory reminder to all those individuals living with HIV/AIDS that they are not alone in their fight.
April 08, 2019
|

How Open Is Too Open for Your Office?
It’s time to end the debate about whether offices should be an open or closed environment. Gensler’s U.S. Workplace Survey provides answers to how the open office should be.
April 01, 2019
|

How Do We Accommodate Traveling Service Animals?
In order to make travel more accessible for all passengers, airports are required to provide relief areas for use by service animals. The definition of a service animal has expanded and contracted over the years and, as such, it can be challenging to understand how to best serve their needs.
March 26, 2019
|

It's Time for Office Amenities to Get to Work
As the office landscape continues to evolve and companies grant their employees more freedom and choice to work where they like (whether inside or outside the office), Gensler's research shows that the amenities with the greatest impact on effectiveness and experience are those that directly support the work needs of individual employees and their teams.
March 22, 2019
|

10 Tips for Success in an Open Plan
Transitioning to an open plan doesn’t have to be intimidating. In fact, if it’s an office layout where you have a range of spaces to support focus and collaboration, you'll likely be even be more effective and productive.
March 20, 2019
|

The Open Office Isn't Dead (Redux)
It’s time for a new narrative around work and the workplace — one that reflects the realities of the needs and desires of today’s workers and the diversity of the modern workforce.
March 19, 2019
|
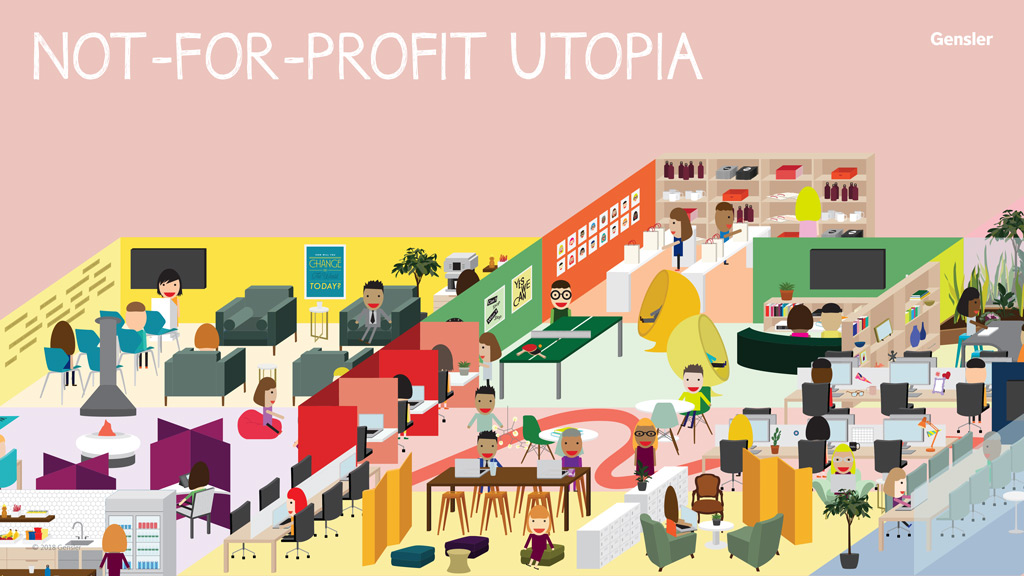
Why Not-For-Profits Deserve a Utopian Workplace
Not-for-profit employees are four times more likely to be motivated by mission than the average employee in another sector. What would their workplace utopia look like?
March 07, 2019
|

The Third Lane: Rethinking Street Design for the 21st Century
What does the explosive growth of shared electric scooters tell us about the changing dynamics of city life? And how can we better shape the city of tomorrow to respond to new modes of mobility?
February 26, 2019
|

Keep it Moving: New Technologies at the Airport Curbside
The disruptive impact that Transportation Network Companies and app-based rides have had on airport curbsides has been significant. While companies such as Uber, Lyft, and Wingz are becoming more commonplace, many airports have been caught off guard. Now they’re scrambling to catch up.
February 18, 2019
|

From Smart Buildings to Intelligent Placemaking
Data and AI are being invisibly woven into everything around us. As we move towards an intelligence economy where data is a raw material, we have an opportunity to take a new approach to design.
February 14, 2019
|

Polycentric Cities: The Future of Sustainable Urban Growth
As we approach a new normal for urban density, the cities that are best positioned for the future are evolving along a decentralized, multi-nodal model.
February 12, 2019
|

If A City Isn’t Smart, Does That Mean It’s Stupid?
The concept of smart cities might be shrewd marketing on the part of tech companies, so what does it mean for a city to truly be “smart”?
February 06, 2019
|

On Climate Change and Hope
Despite rising carbon dioxide emissions, we can still tackle global warming.
January 23, 2019
|
How Will Biometric Screening Change the Airport Environment?
Fueled by science fiction, biometric screening has long been associated with a futuristic society. Today, governmental agencies, airlines, and airport operators are all exploring the technology as a means to both increase security and improve passenger processing.
January 22, 2019
|
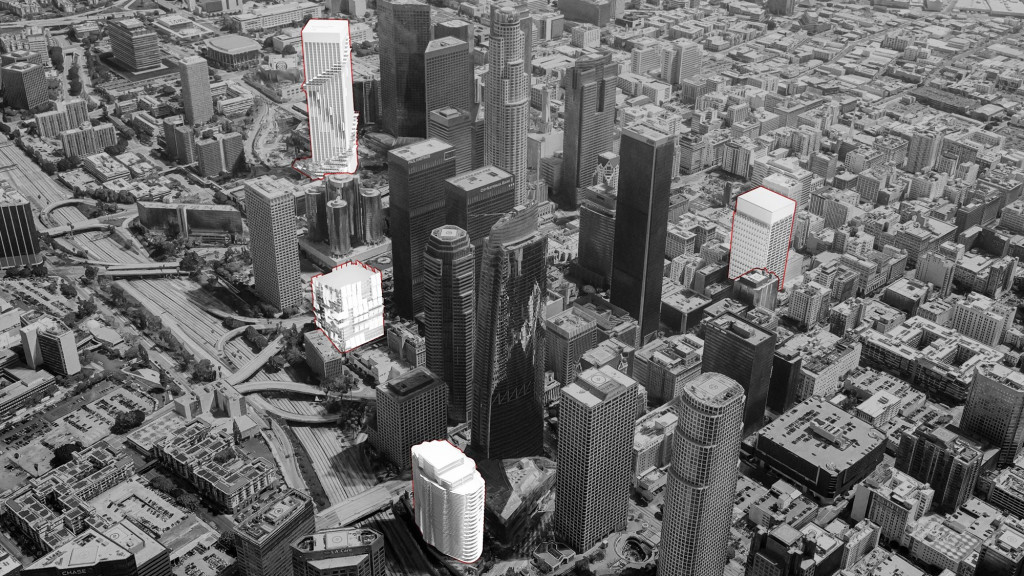
Climate Reprogramming
Façade design is an example where performance, technology, and code changes come together to positively impact the environment; our first target should be existing buildings.
January 10, 2019
|

Creating Transit-Oriented Communities in Los Angeles
Phil Washington of the LA Metro spoke about connecting transit-oriented communities and kicked off a critical shift in the way we think about transportation investments.
January 08, 2019
|

Reimagining the Hotel Lobby as a Vibrant Social Hub
Many of today’s travelers spend more time in the lobby than in their rooms — and, with a mix of hotel guests and locals, today’s lobby feels more like a neighborhood coffee shop than a hotel entry point. Today, the lobby must be a vibrant, 24/7 revenue-generating space designed for a mix of different uses.
January 03, 2019
|

From Railroads to Electric Scooters: How Mobility Shapes the City of Today and Tomorrow
From GPS-enabled electric scooters, to driverless cars, and even aerial ride-share services, disruptive mobility is on the rise. With the explosion of these services, it’s critical that we build a common language of understanding as we shape a vision for the cities of tomorrow.
December 19, 2018
|

Creating a Beautiful, Energy-Efficient Building for Harbin Bank
Harbin Bank’s new headquarters in Beijing is both aesthetically pleasing and high performing. By maximizing natural daylight and energy efficiency, while minimizing harmful particulates, the building serves as a climate-responsive solution and an elegant example for the city.
December 17, 2018
|

What the Math Behind Climate Change Is Telling Us
Global carbon emissions reached a record high in 2018. As the math of climate action suggests a growing gap between countries’ action pledges and their measures to limit global warming, the question for our industry becomes: how do you approach sustainability design in a world where arresting climate change no longer seems possible?
December 14, 2018
|

An Advocate’s Journey: The Role of Design in Enabling Issue Advocacy
Physical space can and should be a catalyst for issue advocacy and it can be the gateway that initially connects people to an issue or cause.
December 12, 2018
|

2018 Gensler Design Excellence Awards
Now in its 19th year, the Gensler Design Excellence Awards (GDEA) program sets a standard that all our design teams can aspire to. Within our global firm of more than 6,000 employees, the annual program is a purposeful tradition that nurtures and elevates our design culture.
December 11, 2018

Improving the Air We Breathe: Design Strategies for Action
Fire and unhealthy indoor air are global issues. What can we do to improve air quality in the environments we design?
November 30, 2018
|

The Costs of Climate Change and the Promise of Resilience
If there’s one clear lesson from the recent National Climate Assessment, it’s that we need to anticipate and prepare for extreme weather-related events, rather than simply react to them. At Gensler, we believe that the building industry has an obligation to help communities prepare while leading the charge against climate change.
November 27, 2018
|

Sorting It Out: The Key to Zero Waste Is in the Bin
If the team at San Francisco International Airport is to reach its zero waste goal in the next three years, the airport's facilities must be able to efficiently sort out renewable or reclaimable materials. But if these items are consistently ending up in the wrong bin, then the point of failure in the system seems obvious: the airport just needs better bins.
November 20, 2018
|

As Wildfires Rage in California, Designing for Resilience Becomes Even More Urgent
The effects of climate change are increasingly evident — and urgent. What can we do to create resiliency and mitigate the impact of these frequent and powerful events?
November 16, 2018
|
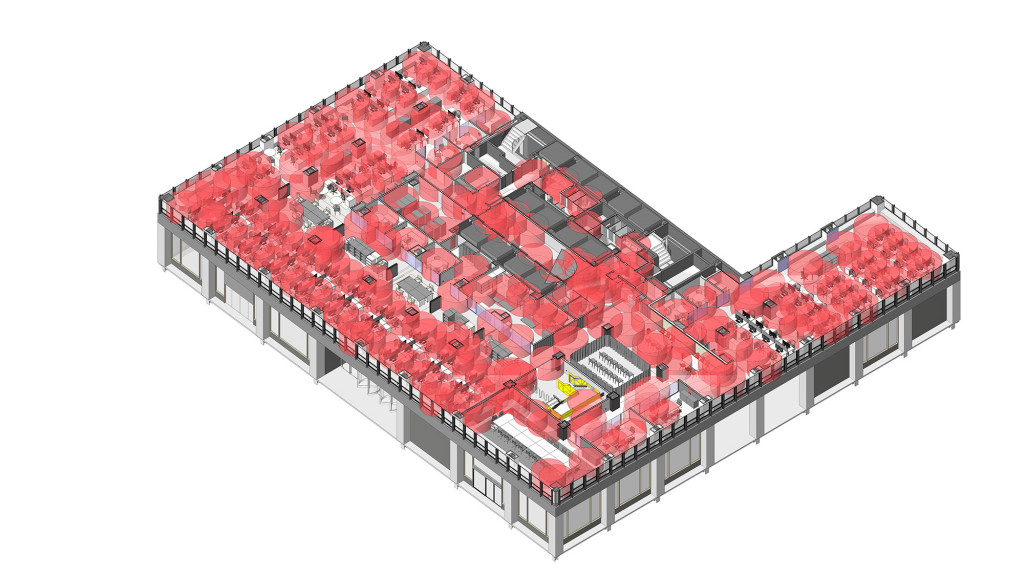
Pairing BIM and Connected Devices to Elevate Design
Designing in an intricate world involves considering numerous factors. Networked devices help measure various aspects in our created spaces.
October 23, 2018
|

How the Built Environment Can Help the Climate Crisis
The design industry has an opportunity to make positive impact in the face of climate crisis — here are 5 steps Gensler is taking to reduce carbon impact.
October 11, 2018
|

City of Hope Honors Gensler With Spirit of Life Award
City of Hope Honors Gensler With Spirit of Life Award
October 10, 2018

Preparing for the Future Now with Resilient Design
As global leaders come together to address how the collective community can help reduce CO2 emissions, we understand our role within this conversation, too.
September 26, 2018

The Smart and the Beautiful Dichotomies in Workplace Design
For tomorrow's workplace, the prime differentiator will be realizing a firm’s cultural promise through the physical form and sequence of its space.
September 05, 2018
|

Red Bull Reenergizes a Warehouse as Their Atlanta Workplace
Southern charm and the high-octane world of Red Bull collide for an enthusiastic atmosphere in their new Atlanta office. The office enhances their employees’ experiences by celebrating its local dedication and passion to its Southern customers.
August 08, 2018
|

The Open Office Isn't Dead
No two employees or companies are exactly alike. It’s a good idea to remind ourselves of these individualities before jumping to any conclusions.
July 26, 2018
|

Will California Lead the Way to Energy Independence?
Global changes are shifting the conversation around energy conservation and climate change from a voluntary, corporate social responsibility goal to a business imperative.
June 18, 2018
|

Designing the First Triple-Certified Green Building in China
Johnson Controls’ Shanghai headquarters incorporated cutting-edge sustainable mechanical, electrical, and plumbing systems, as well as intelligent building features.
June 11, 2018
|

From Fitness to Bowling Alleys: How Commercial Office Buildings Are Differentiating Themselves Through Amenities
Here, we offer five ways that amenities can help developers and building owners attract and secure tenants by appealing to their inhabitants
March 28, 2018
|

But First Let Me Take a Selfie: Designing Sharable Moments
As our lives become more digitally connected, there is not a moment uninterrupted by the desire to post something unique or exciting, leading to an ever-growing demand for photo opportunities to share.
February 26, 2018
|

Gensler Atlanta's Office Expansion: A Co-Creating Environment
When we started thinking about our expansion space for Gensler Atlanta’s office last May, we wanted to build an environment that would continue to inspire a creative culture, where each individual’s ingenuity can be unleashed and turned into works of collective genius.
January 29, 2018
|
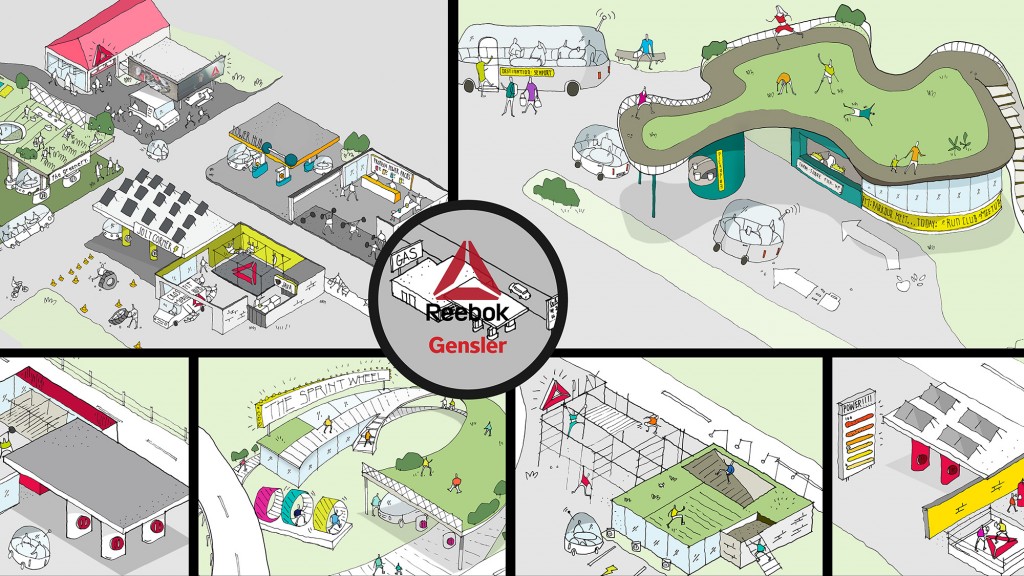
The Gym Of The Future is Closer Than You Think
What do we do when gas stations become obsolete? Turn them into fuel for our bodies instead.
January 17, 2018

How Environmental Graphics can Inspire Culture and Creativity
The big question is, once you secure outstanding talent, how do you keep the creative juices flowing and help employees feel more connected to their company’s culture?
December 11, 2017
|

How Businesses Can Compete on Experience, and Win on Design
Today, the goal of every project we design at Gensler is to make a positive impact to peoples’ experiences.
November 17, 2017
|

Seven Ideas to Create an Inspiring Workplace
Achieving the right kind of workplace is challenging, but the following ideas can change your office from a mundane “greige” environment into something that inspires creativity and innovation.
November 06, 2017
|

Design as an Innovation Super Power
Innovation is an overused word and an underexplored practice.
October 24, 2017
|

The Solutions to Climate Change Are Already at Our Fingertips
Because every project we work on is either part of the problem or part of the solution, we made a commitment to measure the environmental impact of our work, and publish the results to drive discussions about the best ways to make progress in the future.
September 20, 2017
|

Comparing Boma 2010 and 2017 Office Standards
The latest Office Standard provides a uniform basis for measuring rentable area in both existing and new office buildings.
August 30, 2017
|

Wellbeing in the Workplace Has Superpowers
The wellbeing of your employees is a business strategy aimed at increasing productivity, enhancing engagement, and improving overall health and happiness in the workplace.
August 14, 2017

Dear Office Worker, The Future Is Free-Address
Workplaces are shifting from endless rows of cubes to a free-address work environment that allows you to work anywhere and everywhere. You are no longer tethered to an office or a cubicle. Why the shift?
June 20, 2017
|

Are Law Firms Ready to Work Remotely?
The legal industry and most other industries are reshaping their workplaces. The most innovative of the bunch are taking less space and collaborating more.
May 22, 2017
|

Employee Engagement: A Core Business Strategy
Successful business leaders realize that having engaged employees is not an HR program, but a core business strategy.
April 27, 2017
Re-Imagining an American Icon
The Willis Tower is one of the world’s tallest buildings. At ground level, however, something is noticeably absent.
March 29, 2017
|

Human Experience Is the Future of Design
We believe human experience is the future of design. People are the one constant in this era of dramatic technological change, demographic shifts, global volatility and climate change.
February 27, 2017
|

Want to Attract Top Talent? Focus on the Employee Experience
The workplace of the future is more about ‘how’ we work; bringing people together to collaborate, innovate, learn, and socialize.
January 02, 2017
|

Gensler Partners with the City of Bogotá on Community Center Initiative
Gensler Partners with the City of Bogotá on Community Center Initiative
September 01, 2016

A Workplace Designed for the Innovation Economy
The ability to drive new innovation is becoming an essential requirement for organizations to stay competitive today. All the signs point to the same realization… disrupt or be disrupted is the ethos of our time.
July 08, 2016
|

Designing Vibrant Communities
Vibrant communities are the building blocks of our fast-paced, increasingly urban world. To help cities thrive, these communities must be connected, resilient, healthy and inspiring.
February 26, 2016

Delivering Creativity on a Global Scale
Our firm revolves around a shared commitment to design excellence and a culture of entrepreneurial self-sustaining leadership.
December 16, 2015
|

What makes a world-class airport?
Gleaming new terminals are rising in next-generation cities across the globe; and with these come growing expectations of the airport experience. To remain competitive, legacy regional and national airports are asking: What makes for a world-class airport today?
November 13, 2015

Vertical Urbanism and the Livable Cities of Tomorrow
Open spaces – the parks and piazzas that give cities a sense of character and community – are in short supply. To ensure cities remain livable in an urbanizing world, new perspectives on public space are needed. One approach is to look beyond the ground plane.
April 20, 2015

The Rise of Academic Incubators
Gensler is exploring the impact of academic incubators on universities, businesses, and communities, leveraging expertise in workplace and higher education design.
March 16, 2015

What Is the Function of Libraries in Our New Wired World
The desire to work in a physical environment surrounded by other people is why libraries remain important places for studying and performing individual work.
August 29, 2014
|

All Squared Away
22squared’s new office makes a pitch for the ad agency’s creative culture
May 29, 2012

Want more of Gensler’s design insights? Sign up for our dialogue Now newsletters to get regular updates sent directly to your inbox.